Summary
Cotton rats are extremely excitable and have a strong flight-or-fight response. A handling method optimized to reduce the stress of the animals is described which will make cotton rats more accessible as a preclinical model.
Abstract
Oncolytic viruses are a novel anticancer therapy with the ability to target tumor cells, while leaving healthy cells intact. For this strategy to be successful, recent studies have shown that involvement of the host immune system is essential. Therefore, oncolytic virotherapy should be evaluated within the context of an immunocompetent model. Furthermore, the study of antitumor therapies in tolerized animal models may better recapitulate results seen in clinical trials. Cotton rats, commonly used to study respiratory viruses, are an attractive model to study oncolytic virotherapy as syngeneic models of mammary carcinoma and osteosarcoma are well established. However, there is a lack of published information on the proper handling procedure for these highly excitable rodents. The handling and capture approach outlined minimizes animal stress to facilitate experimentation. This technique hinges upon the ability of the researcher to keep calm during handling and perform procedures in a timely fashion. Finally, we describe how to prepare cotton rat mammary tumor cells for consistent subcutaneous tumor formation, and how to perform intratumoral and intraperitoneal injections. These methods can be applied to a wide range of studies furthering the development of the cotton rat as a relevant pre-clinical model to study antitumor therapy.
Introduction
Oncolytic viruses (OV) selectively replicate in tumor cells by exploiting biochemical differences between normal and tumor cells 1,2. There are two types of OVs: those that do not require a mutation to achieve selective oncolysis, referred to as naturally occurring wild-type viruses and those which must be engineered to achieve selective oncolysis. The collection of mutations within a given tumor type determines the nature of the selective growth advantage over normal cells for an OV 2. The safety and benefit of using OVs has been demonstrated in clinical trials 3-7. Despite advancements in the field of oncolytic virotherapy there exist gaps between pre-clinical and clinical results, suggesting that better models are needed to evaluate the antitumor efficacy of OVs.
Bovine herpesvirus type 1 (BHV-1) is a member of the Herpesviridae family, and Alphaherpesviridae subfamily. BHV-1 initiates bovine respiratory disease complex in cattle, manifesting in a wide variety of symptoms resembling a bad cold 8,9. BHV-1 binds attachment and entry receptors used by HSV-1, such as heparan sulfate and nectin-1 10. However, it binds CD155 in the place of nectin-2 10. BHV-1 has a very narrow host range such that it is unable to efficiently enter and initiate replication in normal and transformed murine cells 3,4,10. This makes the use of conventional murine models problematic. The oncolytic capacity of BHV-1 has been demonstrated in vitro11,12. BHV-1 has been shown to initiate replication in and kill human tumor cells from a variety of histological origins, including breast cancer cells and breast cancer initiating cells 11,12. However, the antitumor capacity of BHV-1 must be evaluated in vivo within the context of an immunocompetent host.
Human Adenovirus (Ad), for which there are 57 identified serotypes, most commonly causes respiratory illness in humans. Oncolytic Ad vectors have been evaluated for their antitumor efficacy with several advancing into clinical trials 13-15. Despite promising pre-clinical data, clinical results have fallen short of expectations. Human tumor xenograft models are typically used to study the antitumor efficacy of Ad vectors, although they exhibit attenuated immune responses to the virus 16,17. Furthermore, syngeneic murine models are non-permissive to Ad infection, making the evaluation of host immune responses using these models impractical 17,18.
The host immune system has been identified as the most influential mechanism by which OVs elicit tumor cell death 19. Antitumor responses between tolerized and non-tolerized tumor-associated antigen (TAA) models differ and can greatly impact the success of OV therapy. The HSV-1 OV KM100 (ICP0n212VP16in181420)20,21 elicited tumor regression in 80% of tumor-bearing mice in a murine Polyoma Middle T antigen mammary cancer model 22. However, in HER-2/neu models, the antitumor efficacy of KM100 varied between 20% complete regression in syngeneic mice and tumor stasis in transgenic, HER2-tolerized mice. Together these data highlight the importance of fully evaluating OVs using animal models that best recapitulate the human immune landscape to fully understand what features determine therapeutic success.
The cotton rat (Sigmodon hispidus), indigenous to North and South America, is most commonly used as a model of respiratory syncytial virus infection (as reviewed in 5). Cotton rats are also used in anti-BHV-1 vaccination research as they recapitulate the pathology associated with bovine respiratory disease complex 6,23. Furthermore, BHV-1 infection of cotton rats is immunogenic, inducing sustained mucosal and systemic immune responses 6,23-25. Cell lines have been derived from spontaneous fibrosarcoma and osteosarcomas of the mammary gland (LCRT) and bone (CCRT and VCRT), respectively 26. Cotton rats have been used to evaluate the in vivo efficacy of oncolytic Ad vectors as they are susceptible to Ad infection and exhibit similar pathology to humans 27-29. The use of immunocompromised models for the pre-clinical evaluation of OVs are not only less indicative of clinical responses to therapy but they fail to take into account the role of the immune system in oncolytic virotherapy 30,31. Therefore, the syngeneic and tumor-tolerized cotton rat models of mammary carcinoma and osteosarcoma are relevant models in which to evaluate the pre-clinical efficacy of OVs, such as BHV-1 and Ad which cannot be studied using conventional murine models.
Subscription Required. Please recommend JoVE to your librarian.
Protocol
NOTE: The protocols used have been approved by our institutional Animal Research Ethics Board at McMaster University according to Canadian Council on Animal Care guidelines. Experiments were performed at the McMaster University Central Animal Facility.
1. Culturing LCRT Cells
- Culture LCRT cells in Dulbecco’s modified Eagle’s medium (DMEM) supplemented with 10% fetal bovine serum (FBS), 2 mM L-glutamine, 100 U/ml penicillin and 100 µg/ml streptomycin. Maintain cells in T-150 tissue culture flasks at 37 °C and 5% CO2. Passage cells when they form a 90% confluent monolayer (every 2-3 days, Figure 1).
- Pre-warm 1x phosphate buffered saline (PBS), 1x trypsin and medium in a 37 °C water bath for 10 min prior to splitting the cells.
- Aspirate medium from the flask and rinse cells with 5 ml of 1x PBS.
- After rinsing, aspirate PBS and incubate cells with 2 ml of 1x trypsin until cells dissociate from the flask (~2 min).
- Resuspend cells in 8 ml medium (for a total of 10 ml cell suspension) and gently pipette up and down to break up clumps of cells.
- Maintain cells in a T-150 flask by seeding 1 ml cell suspension into 24 ml medium (for a total of 25 ml per T-150) and rock flask gently from side to side. Maintain cells at 37 °C and 5% CO2 until next split.
2. Assessing Virus Replication and Cytotoxicity in LCRT Cells
- Virus Replication
NOTE: Virus constructs expressing a fluorescent tag, such as green fluorescent protein (GFP), under control of endogenous viral promoters facilitate visualization of virus infection and spread using fluorescence plate readers.- Seed LCRT cells into culture plates, leaving a well for counting. Seed cells such that they will be 80-90% confluent one day later. Use a concentration of 105 cells/ml (100 µl per well) to produce the desired confluency one day later in 96-well flat bottom plates.
- The next day, pre-warm 1x PBS, 1x trypsin, complete and serum-free medium in a 37 °C water bath for 10 min prior to starting the experiment.
- Aspirate medium from the counting well and rinse cells with 5 ml of 1x PBS by rocking it over the surface of the well.
- After rinsing, aspirate PBS and incubate cells with 2 ml of 1x trypsin until cells dissociate from the flask (~2 min).
- Resuspend the cells in the appropriate volume of complete medium to yield a cell density within the countable range using a hemocytometer. To ensure an accurate cell count, thoroughly mix the cell suspension prior to inoculating the hemocytometer by pipetting up and down.
- Determine the volume of virus stock required for infection at the desired multiplicity of infection (MOI).
Required Paque Forming Units (pfu) = number of plated cells * MOI (pfu/cell)
Volume of virus stock required = required pfu / virus stock titer (pfu/ml) - Prepare virus inoculum in serum-free medium in tubes. Mix thoroughly by vortexing or pipetting before adding inoculum to the cells.
- Infect cells for 1 hr at 37 °C, after which apply a maintenance overlay of DMEM + 1% FBS.
- Scan plates one and two days post infection (pi) to visualize GFP fluorescence.
- Virus Cytotoxicity
NOTE: Perform the resazurin cytotoxicity assay under low light conditions as the compound is photosensitive. A well containing medium only should be included to correct for background fluorescence.- Prepare a 5% (v/v) solution of resazurin in 1x PBS. Mix the solution by pipetting.
- Aspirate medium from cells and apply the 5% resazurin solution. Include a well containing medium only to correct for background fluorescence.
- Incubate cells for 30 min at 37 °C, after which read fluorescence using a fluorescence plate reader (excitation 530 nm, emission 595 nm).
- Analyze data relative to uninfected controls correcting for background fluorescence.
3. Housing and Handling
- Housing and Diet
- House cotton rats individually to decrease in-fighting in polycarbonate rat cages containing rodent bedding (1/8” corncob bedding), a section of PVC tubing no longer than 8 inches and nestlets as enrichment (Figure 2).
- Use a securable steel basket to sit overtop of the cage and contain rodent food and a water bottle.
NOTE: This cage setup will allow for safe and easy capture of the animals, with the placement of the enrichment tube against the end of the cage being of the utmost importance.
- Handling
- Handle cotton rats in the morning, prior to rounds by animal facility technicians to avoid exciting them before a procedure.
- During all procedures, wear thick leather gloves for protection.
- As the animals primarily remain in the enrichment tubes, use them to transfer the rats into a new cage during routine cleaning. Alternatively, open the cage slightly to allow the handler to reach their hand in, the animal can then be restrained by scruffing the skin just above the shoulders and pushing down. Practice care not to use excessive force as the animal may bite their tongue.
- Be patient and use a steady hand as the animals have a strong flight-or-fight response and will try to avoid capture by running and jumping out of the cage. Importantly, do not handle animals by the tail as degloving will occur.
- Trap the animals in their enrichments tubes over direct handling. This drastically decreases injuries and escaping.
4. Capture and Anesthesia
- Capture
- Wear thick leather gloves for protection during all procedures.
- Use a large clear plastic container with holes for air and a lid, an anesthetic induction chamber large enough to fit the container and a nose cone fitted to the gas output hose (Figure 3).
- Work in pairs to make the procedure more efficient and to decrease the exposure time of the animals to isoflurane, an inhalation anesthetic. Make sure one researcher is responsible for opening and replacing the steel cover on the cage and the lid of the induction chamber (handler #1) and their associate is responsible for capture of the animal in the tube and transport to the induction chamber (handler #2).
- Place the cage on a flat surface and remove the outer lid. Lift the steel feed tray slightly and slowly maneuver the enrichment tube so it is parallel with the sides of the cage and against the back. If necessary, use an object to maneuver the enrichment tube without opening the cage to avoid agitating the animal (handler #1).
- If the animal becomes agitated and leaves the tube, allow adequate time for the animal to relax and once again settle in the tube (handler #1).
- Slowly and deliberately lift the edge of the steel cover furthest from the enrichment tube, keeping the other end in contact with the cage. Make a space large enough for the plastic container (handler #2).
- In one smooth, quick motion, push the plastic container overtop of the enrichment tube. Maintain contact of the container with the side of the cage, trapping the animal in the tube. Perform steps 4.1.6 and 4.1.7 as quickly as possible (handler #2).
- Remove the steel feed tray and give the plastic container lid to handler #2 (handler #1). Slide the plastic lid between the side of the cage and the container, being mindful of the trapped animal’s appendages in the process. Do not seal the container as this will make the next step more difficult (handler #2).
- Anesthesia
- Make sure the container remains closed and transport the animal to the induction chamber. Quickly place the animal in the chamber and remove the container lid in one fluid motion (handler #2). Open and immediately replace the induction chamber lid (handler #1).
- Turn on the flow of isoflurane to the induction chamber (5 L/min) and monitor the animal for signs of lethargy, at which point quickly slide the animal from the tube and container, removing both from the induction chamber to facilitate gas circulation.
- When the rat is fully anesthetized, move it to the working surface and place the nose and mouth into the nose cone (Figure 3). The rat is fully anesthetized when it is unresponsive to a forceful toe pinch.
- Place vet petrolatum ophthalmic ointment on the animal's eyes to prevent dryness and abrasions. This is an essential step as cotton rats have large eyes that can be prone to infection if injury occurs.
- Carefully monitor and maintain a constant respiration rate and ensure that the animal’s nose remains in the nose cone fitting throughout the procedure. Adjust the flow rate of isoflurane appropriately. The amount of isoflurane required to anesthetize each animal will vary.
- Post-procedure, return the animal to its cage and ensure it regains full mobility and sternal recumbency.
5. Preparation of LCRT Cells for Subcutaneous Tumor Formation
NOTE: One T-150 flask of LCRT (90% confluency) yields approximately 2 x 107 cells. Base the number of T-150 flasks required on the total number of cells needed. Seed extra flasks to ensure the total number of cells required is obtained and to accommodate cells lost during preparation and those needed for extra injections. Keep cells on ice whenever possible to prolong cell viability.
- To harvest cells, aspirate medium from the flask and rinse cells with 5 ml of 1x PBS.
- Aspirate PBS and incubate cells with 2 ml of 1x trypsin until cells dissociate from the flask (~2 min).
- Resuspend cells in 8 ml medium (for a total of 10 ml cell suspension) and gently pipette up and down to break up clumps of cells. Continue to harvest cells from additional flasks.
- Pool all cell suspensions into one conical tube, approximately 4 T-150s per 50 ml conical tube.
- Centrifuge the tube at 160 x g for 10 min at 4 °C.
- Aspirate medium and resuspend the cell pellet in the appropriate volume of PBS (10 ml PBS per T-150) to yield a cell density within the countable range using a hemocytometer. To ensure an accurate cell count, thoroughly mix the cell suspension prior to loading the hemocytometer by pipetting up and down.
- Calculate the total number of cells:
Total number of cells harvested = cell count (cells/ml) x resuspension volume (ml) - Determine the volume of cell suspension required for all injections. Make 2-3 extra doses per experiment. A total of 5 x 105 LCRT cells injected subcutaneously will form palpable tumors within 3-4 days.
Total number of cells required = 5 x 105 cells x total number of doses
Volume cell suspension required (ml) = (total cells required * sum of injection volumes) / (total number of cells harvested) - Pipet the required volume of cell suspension into a conical tube containing PBS and mix thoroughly. Aliquot individual injections (100 µl) into Eppendorf tubes. Maintain tubes on ice during injection procedure.
6. Injections
NOTE: Perform procedures with two researchers, one to perform the injections while the other monitors the animal’s respiration rate and general condition while under anesthesia. Use insulin syringes (29 G x 1/2’, 0.3 ml) for all injections and a new needle for each animal.
- Subcutaneous injections
- Capture and anesthetize the animal (section 4).
- Shave the injection site using clippers. Cotton rat fur is thick and requires a sharp trimmer to get a smooth surface for injections. Clean the injection site with 70% ethanol using a cotton swab and allow it to evaporate completely before proceeding.
- Load syringes (29 G x 1/2’, 0.3 ml) with the cells by drawing up slowly and steadily. If bubbles are evident flick the syringe with some force. Once the bubbles are at the top push the plunger until the liquid is at the top of the needle.
- Lift the skin at the injection site (referred to as skin tenting) and insert the needle bevel side up. Make sure the needle moves freely under the skin to avoid injecting intramuscularly.
- Expel the contents of the syringe evenly and slowly. Withdraw the needle bevel side down.
- Intratumoral injections
- Capture and anesthetize the animal (section 4).
- Clean the injection site with 70% ethanol using a cotton swab and allow it to evaporate completely before proceeding.
- Load syringes (29 G x 1/2’, 0.3 ml) with the virus inoculum by drawing up slowly and steadily while holding the needle in an upright position. If bubbles are evident flick the syringe with some force. Once the bubbles are at the top push then plunger until the liquid is at the top of the needle.
- Insert the needle bevel side up into the tumor and expel the contents of the syringe evenly and slowly while moving the needle in a fan-like pattern, partially withdrawing the needle before each movement to prevent laceration of the tumor. Withdraw the needle bevel side down.
NOTE: Subcutaneous LCRT tumors are fast-growing, reaching approximately 100 mm3 in 5-7 days. Furthermore, necrotic and hemorrhagic centers often form on the surface of the tumor within several days and require careful monitoring (Figure 4).
- Intraperitoneal injections
- Capture and anesthetize the animal (section 4).
- Clean the injection site with 70% ethanol using cotton swabs and allow it to evaporate completely before proceeding.
- Load syringes (29 G x 1/2’, 0.3 ml) with the drug by drawing up slowly and steadily. If bubbles are evident flick the syringe with some force. Once the bubbles are at the top push then plunger until the liquid is at the top of the needle.
- Insert the needle into the right lower quadrant of the abdomen. Pull back on the plunger to ensure that blood or feces are not aspirated, this indicates incorrect placement of the needle. If this occurs, withdraw the needle and prepare a new syringe. When the needle is correctly placed, expel contents of the syringe evenly and slowly.
7. Tumor Excision and Necropsy
- Gather and clean all tools with 70% ethanol prior to euthanasia of the animal.
- Euthanize the animal by the desired method, CO2 inhalation (2 L/min for 5-10 min) is recommended. Examine the animal for any abnormalities in body condition.
- Place the animal in dorsal recumbency on a dissection board and clean the animal with 70% ethanol.
- Use tweezers to lift the skin at the lower abdomen. Cut through the skin and muscle using scissors and make a medial incision running the length of the animal (anus to chin).
- Cut the rib cage by making two cuts, one laterally up the side of the ribcage and one across the sternum to expose the heart and lungs. Examine the lobes of the lung for any metastases 27,29.
- Examine all organs for abnormalities and record any changes in color, size, and consistency. If necessary, incise the organs with a scalpel to examine internal tissues. Specifically, examine the liver, kidneys, spleen and gastrointestinal tract.
- Inspect the lymph nodes for metastases and enlargement 27,29.
- To collect the tumor, make flank incisions above and below the tumor such that the skin can be pulled away from the body with tweezers. While firmly holding the skin with tweezers, use a scalpel to carefully remove the tumor by cutting between the tumor and dermis (Figure 5).
- Immediately place the tumor in a labeled container of 10% neutral buffered formalin.
- Depending on the size of the tumor, allow 1-2 days (≤ 2 mm, small) or 5-6 days (> 2 mm, large) for fixing before preparing sections for histological analysis (Figure 6).
Subscription Required. Please recommend JoVE to your librarian.
Representative Results
Due to the extremely excitable nature of cotton rats, being familiar with and utilizing procedures optimized to reduce the stress of the animals will ease in their use as a pre-clinical animal model. Use of proper handling techniques will also minimize risk to the researcher.
When using cotton rats it is imperative to stay calm. The rats are highly excitable and will attempt to escape their cage. Use of an enrichment tube and nestlets will minimize escape attempts. Figure 2 shows optimal cage setup to aid in capture of cotton rats, including placement of the enrichment tube. Furthermore, work in a small room if possible to aid in recapture. If escape occurs, wait for the animal to calm down and remain stationary, then cover it with the clear capture container or cover with gloved hands, being careful not to use excessive force.
In contrast to a mouse, the cotton rat has an elongated snout which requires a different nose fitting to deliver the anesthetic gas. Figure 3 depicts a nose cone engineered to properly fit a cotton rat and maximize delivery of isoflurane. Using a rubber membrane as a fitting may result in trauma to the nose of the rat.
If possible obtain discard animals (those not needed by other researchers, cotton rats or otherwise) to practice injection techniques prior to attempting them on the rats. This will allow the researcher to gain familiarity with needles and how to safely handle them. Insulin syringes are suggested for injections in cotton rats as their skin is thick and tough in comparison to a mouse. However, a larger needle (21 G x 1’) can be used for the injection of tumor cells to avoid loss of cell viability due to cell shearing during injection. Safety precautions should be followed, such as not recapping needles and proper disposal into a sharps container.
The injection of viable tumor cells is important for proper tumor formation. Figure 1A shows a healthy monolayer of LCRT cells which can be prepared for injection into cotton rats. In comparison Figure 1B shows LCRT cells which have low viability and should not be used for injections. It is important to verify tumor cell viability using a method such as Trypan blue staining when counting cells for injections.
The tumors formed from LCRT cells are fast-growing and necrotic centers often form (Figure 4A). As such, tumor formation should be monitored carefully to avoid ulceration (Figure 4B). If ulceration occurs the animal should be sacrificed to avoid infection and possible death from sepsis.
The effects of anti-tumor treatments are often best examined through histological analysis. This requires excision of the tumor post mortem. Maintaining tumor tissue integrity will result in a sample which is a more accurate representation of the tumor in vivo. Figure 5 shows an excision technique by which the tumor is carefully separated from surrounding tissue using a scalpel and tweezers. Removing the tumor by pulling it by force from the surrounding tissue using tweezers may rupture the tumor or disrupt tumor tissue integrity, impacting proper histological analysis. The dense and highly vascularized structure of the tumor, as seen in Figure 6, is maintained by this excision technique. This is important in analysis of treatments which affect tumor vasculature, as is the case with many OVs.
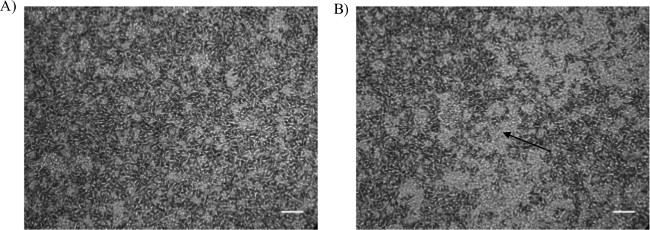
Figure 1: Bright-field microscopy image of LCRT Cells. (A) Phenotype of healthy (~90% viable) LCRT cells ready for preparation for injection into cotton rats. (B) Undesirable phenotype of LCRT cells not fit for injection. Rounded cells are dead or dying (indicated by an arrow). Images were captured at 10X magnification; scale bar = 1 mm.

Figure 2: Example of cage setup for ease of capture of cotton rats. Optimal placement of enrichment tube against the end of the cage and inclusion of nestlets aids in animal capture.

Figure 3: Anesthesia nose cone fitting for delivery of isoflurane to anesthetized cotton rats. Manufactured nose cone fits elongated snout of cotton rat to ensure accurate delivery of isoflurane gas without trauma to nose.

Figure 4: Necrotic tissue on a subcutaneous LCRT tumor. (A) Early stages of necrosis of tumor tissue. The animal should be carefully monitored to avoid progression to (B) fully open ulceration. The animal should be sacrificed if tumor ulcerates as infection and sepsis can result.

Figure 5: Excision of a subcutaneous LCRT tumor for histology. The subcutaneous tumor on the flank of a cotton rat is carefully removed from the skin using a scalpel to maintain tumor tissue integrity, thus providing a better representation of tumor architecture for histological analysis.

Figure 6: Histological tissue section from a subcutaneous LCRT tumor. The morphology of LCRT tumor tissue examined using paraffin-embedded sections stained with hematoxylin and eosin (H&E). Image was captured at 20X magnification; scale bar = 1 mm.
Subscription Required. Please recommend JoVE to your librarian.
Discussion
Cotton rats are highly excitable and have a strong flight response. Therefore, special care should be taken to minimize any undue stress on the animal. The cage setup described will allow for safe and easy capture of the animals, with the placement of the enrichment tube being of the utmost importance. When setting up cages, ensure that the enrichment tubes meet the size and shape requirements, and are placed in proper orientation in the cage. It is also important to ensure that any technicians who might be aiding in animal maintenance are informed of the specific requirements for housing. Taking these precautions will reduce agitation of the animal prior to performing procedures. It is also advisable that procedures be performed in the morning, before any handling by technicians or animal facility staff. Commencing procedures with calm animals will aid in their capture and handling.
The use of nestlets is highly recommended. In the wild, these rodents make their nests out of cotton so they are more comfortable when given the option to build them in their cages. A nest can also aid in animal capture, such that the presence of the animal in the enrichment tube may no longer be required. In this case, the plastic container may be placed directly on top of the animal from above. This action is of particular use as an experiment progresses as the rats may adapt to avoid the traditional capture method.
When handling cotton rats it is of the utmost importance that the researcher remain calm and make deliberate movements. These animals can sense unease and will respond to the perceived emotional state of the handler. Wearing thick leather gloves, following the procedures as described and approaching them calmly and with confidence will protect from bite injuries.
There are conflicting reports in the literature regarding the response of cotton rats to anesthetics 26,32. Sedation of cotton rats for extended periods of time using isoflurane is not recommended 32. We have found that, with careful monitoring, animals can be sedated using isoflurane for approximately 15-20 minutes without adverse effects. In our experience the rats respond rapidly to isoflurane and are fully sedated within several minutes. Likewise, waking occurs in less than a minute in most cases. However, anesthetizing an animal under intense stress alters their response to isoflurane, such that during waking they experience a lack of hind limb motor control and will stumble around the cage. This effect does not appear to have any lasting impact as the animal can execute proper motor control within several minutes of recovery.
When preparing the LCRT cells for tumor injections, it is imperative that the cells be kept on ice whenever possible to prolong viability. Mix the cells with a large bore pipet to avoid shearing the cells. Furthermore, to ensure that all tumors grow at a similar rate we recommend staggering the preparation of multiple cell suspensions when more than five animals are being injected. This will avoid slower growth of tumors in animals injected last due to decreased viability of the LCRT cells.
Excising the tumor tissue from the skin using a scalpel better maintains the tumor architecture and vasculature for histology in comparison to using tweezers to pinch the tumor from the skin. Although perfusion with phenobarbital will best preserve tissues for histopathology, obtaining a license for barbiturates was a limiting factor and was not performed. Thus, necropsies were performed immediately following euthanasia to preserve tissues. In our experience, this allowed for an accurate assessment of the pathology associated with our treatment.
Overall, the major limiting factor is the requirement for two researchers for handling procedures. Although the procedures can be performed by one handler, the process is greatly facilitated, and the stress of the animals significantly reduced, using two handlers. These procedures require practice and careful planning. Allow sufficient time to carry out methods calmly and deliberately. There exists significant stigma about the aggressive nature of these animals and the difficulty in their handling. This article serves to make these animals more accessible to researchers by detailing a simple, established handling method that effectively minimizes stress and injury to both the researcher and the animals. Using the methods we have described, cotton rats represent an excellent animal model for the study of many immune therapies, including oncolytic virotherapy.
Subscription Required. Please recommend JoVE to your librarian.
Disclosures
The authors acknowledge there are no financial conflicts of interest related to this research.
Acknowledgments
Breanne Cuddington holds a fellowship from the Canadian Breast Cancer Foundation. This work was sponsored by operating grants from the Cancer Research Society and the Canadian Cancer Society Research Institute (formerly the Canadian Breast Cancer Research Alliance). We thank Ann Tollefson (Saint Louis University School of Medicine) for LCRT cells and Dr. Kathleen Delaney and Marion Corrick for technical assistance with cotton rat housing and sedation.
Materials
| Name | Company | Catalog Number | Comments |
| Dulbecco’s modified Eagle’s medium | Gibco | 11965-092 | May use any brand |
| 1X Phosphate Buffered Saline | Can prepare in lab, filter to sterilize | ||
| 200 mM L-glutamine | Gibco | 25030164 | May use any brand |
| 100x Antibiotic-Antimycotic | Gibco | 15240-062 | May use any brand |
| Fetal bovine serum | Quality Biological Inc. | 110-001-101HI | May use any brand |
| T-150cm2 tissue culture flask | Fisher Scientific | 14-826-80 | May use any brand |
| 1X TypLE Express | Life Technologies | 12604-013 | |
| 12-well cell culture plate, flat bottom | Fisher Scientific | 08-772-29 | May use any brand, must be tissue culture treated |
| alamarBlue | Life Technologies | DAL1025 | May use an alternative reagent for determination of cell viability |
| 8640 Teklad 22/5 Rodent diet | Harlan | 8640 | |
| 1/8” corncob rodent bedding | Harlan | 7092 | |
| Nestlets | Ancare | - | Made of pulped virgin cotton fiber, dust-free and autoclavable |
| 50 mL Conical tubes | Fisher Scientific | 14-432-22 | May use any brand, must be sterile |
| Isoflurane USP, 99.9 %, inhalation anesthetic | Pharmaceutical Partners of Canada Inc. | M60302 | |
| 70% Ethanol | Can prepare in lab | ||
| 10 % Neutral Buffered Formalin | Sigma-Aldrich | HT501128 | May use any brand |
| NAPCO NapFlow 1200 Class II A/B3 Biosafety Microbiological Safety Cabinet (cell culture hood) | NAPCO | Model used not currently available | May use any brand |
| Thermo Fisher Scientific Precision Heated Water Bath | Fisher Scientific | Model used not currently available | May use any brand |
| Name | Company | Catalog Number | Comments |
| Reichert Bright-line Hemacytometer | Sigma-Aldrich | Z359629 | May use any brand |
| Typhoon Trio BioAnalyzer | GE Healthcare Life Sciences | Model used not currently available | May use any fluorescence plate reader |
| Tecan Safire2 Multi-detection Microplate Reader | Tecan | Model used not currently available | May use any fluorescence plate reader |
| Allegra 6R benchtop centrifuge | Beckman Coulter | 366816 | May use any brand |
| Table Top Anaesthesia machine | VetEquip | Model used not currently available | May use any brand, must be portable |
| Wahl Peanut Mini Clippers | Wahl | May use any brand of small clippers | |
| Insulin syringes 29 G x 1/2', 0.3 mL | BD | 329464 | May use any brand. Insulin syringes are recommended as they make injections easier through the rat’s tough skin. |
| Cotton swabs | MedPro | 018-425 | May use any brand |
| Sharp-Pointed Dissecting Scissors | Fisher Scientific | 8940 | May use any brand |
| Dissecting Tissue Forceps | Fisher Scientific | 13-812-41 | May use any brand |
References
- Cervantes-Garcia, D., Ortiz-Lopez, R., Mayek-Perez, N., Rojas-Martinez, A. Oncolytic virotherapy. Ann Hepatol. 7 (1), 34-45 (2008).
- Vaha-Koskela, M. J., Heikkila, J. E., Hinkkanen, A. E. Oncolytic viruses in cancer therapy. Cancer Lett. 254 (2), 178-216 (2007).
- Abril, C., et al. Both viral and host factors contribute to neurovirulence of bovine herpesviruses 1 and 5 in interferon receptor-deficient mice. J Virol. 78 (7), 3644-3653 (2004).
- Nakamichi, K., Matsumoto, Y., Otsuka, H. Defective infection of bovine herpesvirus 1 in non-permissive murine cells. J Vet Med Sci. 63 (10), 1139-1142 (2001).
- Boukhvalova, M. S., Blanco, J. C. The cotton rat sigmodon hispidus model of respiratory syncytial virus infection. Curr Top Microbiol Immunol. 372, 347-358 (2013).
- Papp, Z., Babiuk, L. A., Baca-Estrada, M. E. Induction of immunity in the respiratory tract and protection from bovine herpesvirus type 1 infection by different routes of immunization with recombinant adenovirus. Viral Immunol. 11 (2), 79-91 (1998).
- Hughes, T. C. R., Lilley, C. E., Ponce, R., Kaufman, H. L. Critical analysis of an oncolytic herpesvirus encoding granulocyte-macrophage colony stimulating factor for the treatment of malignant melanoma. Journal of Oncolytic Virotherapy. 3, 11-20 (2014).
- Jones, C., Chowdhury, S. A review of the biology of bovine herpesvirus type 1 (BHV-1), its role as a cofactor in the bovine respiratory disease complex and development of improved vaccines. Anim Health Res Rev. 8 (2), 187-205 (2007).
- Jones, C., Chowdhury, S. Bovine herpesvirus type 1 (BHV-1) is an important cofactor in the bovine respiratory disease complex. Vet Clin North Am Food Anim Pract. 26 (2), 303-321 (2010).
- Hushur, O., Takashima, Y., Matsumoto, Y., Otsuka, H. Restriction of bovine herpesvirus 1 (BHV-1) growth in non-permissive cells beyond the expression of immediate early genes. J Vet Med Sci. 66 (4), 453-455 (2004).
- Cuddington, B. P., Dyer, A. L., Workenhe, S. T., Mossman, K. L. Oncolytic bovine herpesvirus type 1 infects and kills breast tumor cells and breast cancer-initiating cells irrespective of tumor subtype. Cancer Gene Ther. 20 (5), 282-289 (2013).
- Cuddington, B. P., Mossman, K. L. Permissiveness of Human Cancer Cells to Oncolytic Bovine Herpesvirus 1 Is Mediated in Part by KRAS Activity. J Virol. 88 (12), 6885-6895 (2014).
- Small, E. J., et al. A phase I trial of intravenous CG7870, a replication-selective, prostate-specific antigen-targeted oncolytic adenovirus, for the treatment of hormone-refractory, metastatic prostate cancer. Mol Ther. 14 (1), 107-117 (2006).
- Freytag, S. O., et al. Phase I study of replication-competent adenovirus-mediated double suicide gene therapy for the treatment of locally recurrent prostate cancer. Cancer Res. 62 (17), 4968-4976 (2002).
- Benjamin, R., Helman, L., Meyers, P., Reaman, G. A phase I/II dose escalation and activity study of intravenous injections of OCaP1 for subjects with refractory osteosarcoma metastatic to lung. Hum Gene Ther. 12 (12), 1591-1593 (2001).
- Prince, G. A. The Cotton Rat in Biomedical Research. Animal Welfare Information Center Newsletter. 5 (2), Available from: http://www.nal.usda.gov/awic/newsletters/v5n2/5n2princ.htm 3-5 (1994).
- Tsai, J. C., Garlinghouse, G., McDonnell, P. J., Trousdale, M. D. An experimental animal model of adenovirus-induced ocular disease. The cotton rat. Arch Ophthalmol. 110 (8), 1167-1170 (1992).
- Ginsberg, H. S., et al. A mouse model for investigating the molecular pathogenesis of adenovirus pneumonia. Proc Natl Acad Sci U S A. 88 (5), 1651-1655 (1991).
- Russell, S. J., Peng, K. W., Bell, J. C. Oncolytic virotherapy. Nat Biotechnol. 30 (7), 658-670 (2012).
- Mossman, K. L., Saffran, H. A., Smiley, J. R. Herpes simplex virus ICP0 mutants are hypersensitive to interferon. J Virol. 74 (4), 2052-2056 (2000).
- Mossman, K. L., Smiley, J. R. Herpes simplex virus ICP0 and ICP34.5 counteract distinct interferon-induced barriers to virus replication. J Virol. 76 (4), 1995-1998 (2002).
- Hummel, J. L., Safroneeva, E., Mossman, K. L. The role of ICP0-Null HSV-1 and interferon signaling defects in the effective treatment of breast adenocarcinoma. Mol Ther. 12 (6), 1101-1110 (2005).
- Papp, Z., Middleton, D. M., Mittal, S. K., Babiuk, L. A., Baca-Estrada, M. E. Mucosal immunization with recombinant adenoviruses: induction of immunity and protection of cotton rats against respiratory bovine herpesvirus type 1 infection. J Gen Virol. 78 (11), 2933-2943 (1997).
- Papp, Z., Babiuk, L. A., Baca-Estrada, M. E. The effect of pre-existing adenovirus-specific immunity on immune responses induced by recombinant adenovirus expressing glycoprotein D of bovine herpesvirus type 1. Vaccine. 17 (7-8), 933-943 (1999).
- Mittal, S. K., et al. Induction of systemic and mucosal immune responses in cotton rats immunized with human adenovirus type 5 recombinants expressing the full and truncated forms of bovine herpesvirus type 1 glycoprotein gD. Virology. 222 (2), 299-309 (1996).
- Steel, J. C., et al. Syngeneic Cotton Rat Cancer Model for Replicating Adenoviral Vectors. Molecular Therapy. 13 (1), 123 (2006).
- Toth, K., et al. Cotton rat tumor model for the evaluation of oncolytic adenoviruses. Hum Gene Ther. 16 (1), 139-146 (2005).
- Toth, K., Spencer, J. F., Wold, W. S. Immunocompetent, semi-permissive cotton rat tumor model for the evaluation of oncolytic adenoviruses. Methods Mol Med. 130, 157-168 (2007).
- Steel, J. C., et al. Immunocompetent syngeneic cotton rat tumor models for the assessment of replication-competent oncolytic adenovirus. Virology. 369 (1), 131-142 (2007).
- Workenhe, S. T., et al. Immunogenic HSV-mediated oncolysis shapes the antitumor immune response and contributes to therapeutic efficacy. Mol Ther. 22 (1), 123-131 (2014).
- Sobol, P. T., et al. Adaptive antiviral immunity is a determinant of the therapeutic success of oncolytic virotherapy. Mol Ther. 19 (2), 335-344 (2011).
- Prince, G. A. The Cotton Rat in Biomedical Research. Animal Welfare Information Center Newsletter. 5 (2), http://www.nal.usda.gov/awic/newsletters/v5n2/5n2princ.htm (1994).



