Summary
We describe a surgical procedure in an anesthetized rat model for determining the muscle tone and viscoelastic properties of the tongue. The procedure involves specific stimulation of the hypoglossal nerves and application of passive Lissajous force/deformation curves to the muscle.
Abstract
The tongue is a highly innervated and vascularized muscle hydrostat on the floor of the mouth of most vertebrates. Its primary functions include supporting mastication and deglutition, as well as taste-sensing and phonetics. Accordingly, the strength and volume of the tongue can impact the ability of vertebrates to accomplish basic activities such as feeding, communicating, and breathing. Human patients with sleep apnea have enlarged tongues, characterized by reduced muscle tone and increased intramuscular fat that can be visualized and quantified by magnetic resonance imaging (MRI). The abilities to measure force generation and viscoelastic properties of the tongue constitute important tools for obtaining functional information to correlate with imaging data. Here, we present techniques for measuring tongue force production in anesthetized Zucker rats via electrical stimulation of the hypoglossal nerves and for determining the viscoelastic properties of the tongue by applying passive Lissajous force/deformation curves.
Introduction
The tongue provides essential support for mastication, deglutition, taste-sensing and speaking. The presence of extrinsic and intrinsic musculature, with distinct innervation and anatomy/function, accounts for the uniqueness of this muscular hydrostat. Recent advances in imaging techniques have provided a more detailed view of its complex anatomy1. Decreased tongue functionality, tongue atrophy, dysphagia, and speech impediments are also common manifestations of myopathic conditions such as Parkinson2, Amyotrophic Lateral Sclerosis (ALS)3, Myotonic Dystrophy (MD)4 and other myopathies.
Changes in muscle composition associated with common disease states affect the mechanical and viscoelastic properties of the tongue. For example, functional analysis of tongue force has uncovered changes in contractile properties associated with aging5,6, hypoxia7,8 and obesity9,10. In the case of muscular dystrophy, increased fibrosis leads to higher muscle stiffness, which translates to lower compliance to deformation when a Lissajous deformation protocol is applied11. Conversely, changes in muscle fat content, like those documented in obese patients, alter both metabolic12 and mechanical properties of skeletal muscle13,14 and are predicted to increase muscle compliance to deformation. Increased tongue fat also correlates with the development of obstructive sleep apnea (OSA) in humans17 by increasing tongue volume to the point of partial upper airway occlusion (apnea)15,16. Similarly to humans, tongue fat infiltration has been documented in obese Zucker rats10, suggesting that this model is a valuable tool for studying the effects of fat infiltration on tongue physiology.
Measuring tongue force requires delicate surgical techniques to isolate and bilaterally stimulate the hypoglossal nerves17,18. Such techniques have been previously described in rats5,17,19,20, rabbits21 and humans22,23, yet with limited visual aids to the investigator. Due to its highly technical nature, the availability of a detailed protocol would significantly improve the accessibility and reproducibility of this technique. The goal of our experimental paradigm is to illustrate a valid and reliable technique for measuring strength and viscoelastic properties of the tongue in a rat model. To accomplish this, the rat is anesthetized, the hypoglossal nerves are exposed and the trachea is cannulated to ensure free access to the animal's tongue. A suture loop then connects the tip of the tongue to a force transducer, capable of controlling both force and length, while two bipolar hook electrodes stimulate the hypoglossal nerves to induce contraction of the tongue. After the force measurement is completed, the length-controlling capabilities of the force transducer are used to rapidly change the length of the tongue, according to a sine-wave protocol with fixed amplitude (Lissajous curves), duration and frequency, allowing one to derive its viscoelastic properties11,24. The protocol will guide the investigator through the dissection steps, the positioning of the animal on the experimental platform, placement of electrodes, and finally to the acquisition and analyses of the force and viscoelasticity data.
Subscription Required. Please recommend JoVE to your librarian.
Protocol
All the procedures including animal subjects have been approved by Institutional Animal Care and Use Committee (IACUC) of the University of Pennsylvania (Protocol number 805822). The described procedure is terminal and does not require the utilization of aseptic conditions or pharmaceutical grade products.
1. Surgical Procedures

Figure 1: Surgical Procedures.
(A) Surgical plan demarcation. The red dashed line indicates the area of the incision. Two black lines indicate the position of the jaw, while the bottom black line marks the position of the thorax. The blue line indicates the hyoid bone. (B) Exposure of the posterior belly of the digastric muscle (arrows) after blunt dissection of fat tissue, the sublingual and submaxillary glands. (C) Resection of the posterior belly of the digastric muscle (dashed green line) to expose the hypoglossal nerve (white arrow). (D) The hypoglossal nerve (white arrow) is cleared from the surrounding fascia. (E) The trachea is exposed by gently pulling apart the smooth muscle around it (the green arrows indicate the direction of the force applied), and lifted (F) to prepare for intubation. The star indicates the tongue's insertion at the hyoid bone. The green dashed line marks the point of incision for the intubation. The white arrow indicates the loose knot prepared to secure the cannula in place once inserted. (G) Incision of the trachea for cannulation. (H) The tracheal cannula is inserted and secured in place with a square knot. (I) Application of the suture to the tongue. Please click here to view a larger version of this figure.
- Anesthesia and preparation for surgery
- Place the rat in the induction chamber with 4% isoflurane anesthesia.
- Lay the animal supine over a heat source and maintain anesthesia with 1 - 3% isoflurane from a nosecone, ensuring a respiratory rate of at least 70 breaths per minute.
- Shave the neck area with an air-clipper and hair removal cream. When using the hair removal cream, spread the cream with a cotton-tipped applicator until the fur is removed. Prolonged exposure to hair removal cream can cause irritation of the skin.
- Clean the surgical field with 70% alcohol (Figure 1A).
- Check the animal's breathing pattern and reflexes (lack of a toe pinch reflex) before proceeding with the initial incision. The continuous monitoring and assessment of the depth of anesthesia is essential (record respiratory rate and lack of reflexes every 10 min); the animal needs to be under a deep, surgical plane of anesthesia during the entire procedure.
- Hypoglossal Nerves Identification
- Open the surgical field with a pair of operating scissors by resecting and removing the skin as indicated by the red-dotted line in Figure 1A.
- Blunt dissect through any fat tissue, the sublingual and submaxillary glands and the muscle layer surrounding the trachea.
NOTE: Be conservative during the dissection. Use blunt dissection whenever possible and be careful not to damage the blood vessels of the neck. - Identify the posterior belly of the digastric muscle (PD) lateral to the trachea (Figure 1B - white arrows). The hypoglossal nerve runs under this muscle (Figure 1C - white arrow). With the electrocautery, resect the PD proximal to the hyoid bone (Figure 1C - dashed line).
NOTE: Do not let the nerve or the tissue around it become dry. Add a drop of mineral oil on the nerve to protect it. To avoid muscle contraction due to field propagation of the stimulus from the electrodes, carefully cauterize the muscle tissue in the possible contact sites around the nerve. - Using a pair of fine forceps, dissect the hypoglossal nerve from the surrounding fascia. With the help of a hook, make sure that at least 3 mm of the nerve are available for the connection of the bipolar electrode (Figure 1D).
- Using micro hemostatic forceps, crush the hypoglossal nerve as distally from the hyoid bone (Figure 1D - white arrow) as possible to avoid retrograde propagation of the stimulus. Crush the nerve by applying pressure on it with the micro hemostatic forceps for 5 s. When the hemostat grasps the nerve, a brief twitch at the base of the tongue should be visible.
- Repeat the procedure for the other side.
- Tracheal intubation
- Expose the trachea by gently separating the surrounding smooth muscles by blunt dissection (Figure 1E - as indicated by the green arrows).
NOTE: Be conservative and use preferentially blunt dissection. Compare the diameter of the cannula with that of the trachea. The cannula should fit correctly in the trachea and should remain stably inserted after being sutured as described in steps 1.3.2 through 1.3.5. - Gently lift the trachea using a pair of suture-tying forceps and pass a 4-0 suture underneath it, close to the thorax. Tie an initial loose knot between the 6th and the 7th ring from the larynx (Figure 1F - white arrow). This knot will be closed once the cannula is inserted in order to hold it in place.
- Slide the stem of a transfer pipette (lubricate the pipette with mineral oil to facilitate the insertion) under the trachea to lift it and facilitate the insertion of the cannula (IV 14 g x 3.25" cannula).
- Cut a small incision between the 4th and 5th rings from the larynx (Figure 1G - white arrow). After the first incision, the opening will tend to spread, therefore be conservative when making the initial cut in order to avoid the complete resection of the trachea.
NOTE: Before performing the incision of the trachea, make sure the cannula is ready and the anesthesia delivery is on. - Start the anesthesia administration through the cannula and insert it gently into the incision, advancing gently inside the trachea the length of approximately 5 rings. Secure the cannula in place with the suture, to create an airtight seal (Figure 1H).
NOTE: Ensure that no fluid enters the nicked trachea in order to avoid suffocation. Once the trachea is incised, the animal will be breathing room air. It is therefore important to quickly insert the cannula so that the delivery of the anesthesia is maintained. When/if moving the animal, monitor the correct position of the cannula in the trachea. - Gently remove the animal from the nosecone.
NOTE: The use of injectable anesthetics instead of isoflurane may simplify the procedure by eliminating the need for tracheal intubation and clearing the experimental workspace from excess tubing.
- Expose the trachea by gently separating the surrounding smooth muscles by blunt dissection (Figure 1E - as indicated by the green arrows).
- Tongue suturing
- Soak a 20 cm long piece of 5/0 suture (we suggest Silk, black braided) in PBS.
- While holding the mouth of the rat open, gently hold the tip of the tongue with the suture-tying forceps.
- Pass the suture medially through the tip of the tongue (Figure 1I - white arrow) paying attention to keep the tongue moist with saline to avoid potential tissue damage.
- Tie a loop approximately 4 cm-wide (the diameter can change based on the distance between the animal and the force transducer).
NOTE: Ensure the suture and the tongue are wet to facilitate the insertion and avoid unnecessary lesions of the tissue.
2. Experimental Setup

Figure 2: Positioning and Securing the Animal.
(A) The mouse is positioned on the experimental platform. The jaw is secured and the mouth maintained open by the application of vertical tension (green arrow). The suture loop is connected to the force transducer (white arrow). (B) The electrodes are connected. (C) Each electrode, mounted on a micromanipulator, is stably connected to the nerve. The inlay shows the termination of the hook electrode. (D) The optimal length of the tongue is measured with a Vernier caliper, from the insertion at the level of the hyoid bone to the tip of the tongue. In this picture, the electrodes were removed for clarity. Please click here to view a larger version of this figure.
Note: Position the animal supine on the heated tray of the apparatus, using the following securing measures to avoid movement during the experiment.
- Secure the nose of the rat to the tray with a plastic-coated metallic twist-tie directly connected to the heated platform (Figure 2A, 2B).
- Maintain the rat's mouth opened by applying vertical tension (use a 3 way-swivel tied to 9 kg test monofilament line and hold in place with a camera stick) (Figure 2A - green arrow).
NOTE: An alternative approach to stabilizing the rat is using a rodent mouth gag or a custom modification of it. It is essential that the mouth is maintained open and stable to avoid movements of the neck which could affect the quality of the measurements. - Connect the suture loop to the force transducer (Figure 2A - white arrow).
- Using surgical tape, immobilize the limbs and the abdomen of the rat to limit movements during the stimulations.
- Apply the two stimulating hook bipolar electrodes to the dissected hypoglossal nerves, proximally to the crush site (Figure 2C).
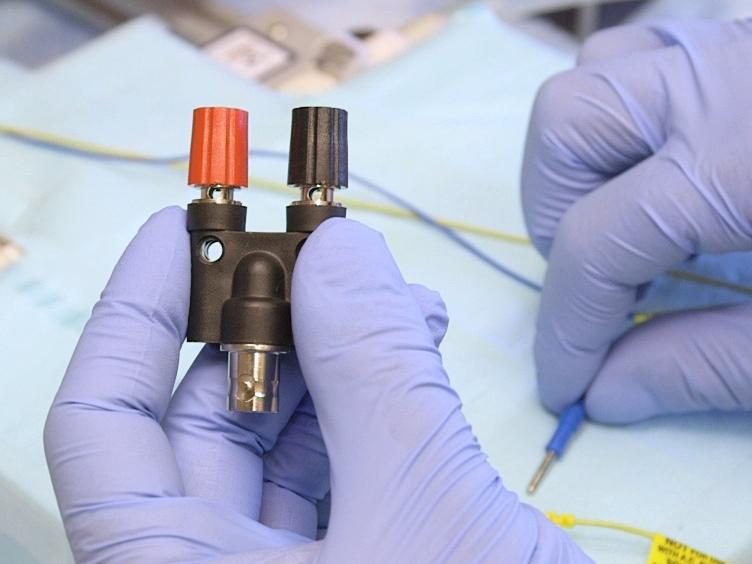
- Use stimulating bipolar electrodes custom made from a pair of surgical-grade steel 29 gauge needle electrodes, held together at a distance of 2 mm from each other using a plastic support (here, we used two 1-mL serological pipettes taped together).
- Bend the tips of the needle electrodes to a hook shape small enough to form a stable contact with the nerve (~1 mm diameter) (Figure 2C - inlay).
- Connect the two wires of each electrode to a stackable double binding post with banana jack x BNC jack, and then connect to the stimulator module of an in situ Muscle Test System (Table 3) using a BNC splitter.
NOTE: Ensure the animal is stable and that the neck and tongue are aligned to the force transducer lever. Continue monitoring the respiratory rate and ensure that the restraints do not interfere with the respiration.
3. Optimal Length (L0) and Maximal Isometric Force Determination
- Adjust the length of the tongue gradually and apply isometric twitch stimulations until a maximal force is obtained.
- Define L0 as the length at which the isometric twitch force (Table 1) is maximal, and record for the subsequent normalization of the force measurements, as it changes for every animal. Using a Vernier caliper, measure the tongue length from the insertion at the level of the hyoid bone (Figure 2D) to the tip of the tongue.
NOTE: The correct positioning of the electrodes is essential to ensure optimal contact with the nerves. Optimal positioning should exert similar and additive forces when stimulating one of the two nerves or both, respectively.
- Define L0 as the length at which the isometric twitch force (Table 1) is maximal, and record for the subsequent normalization of the force measurements, as it changes for every animal. Using a Vernier caliper, measure the tongue length from the insertion at the level of the hyoid bone (Figure 2D) to the tip of the tongue.
- Before starting the experiment, connect both the electrodes to the stimulator and administer a test tetanic stimulation (Table 1). During this contraction, monitor the animal to ensure that the position is stable, and check for unwanted visible contractions of the neck muscles.
- Measure isometric force by applying a twitch followed after 20 s by a tetanic stimulation. Repeat the stimulations 3 times allowing 4 min recovery between stimulation cycles (a cycle includes one twitch and one tetanic stimulation), and record the maximal twitch and tetanic forces.
- Maintain the tongue wet at all times by applying a few drops of PBS between contractions.
NOTE: If neck muscles contract, carefully change the positioning of the electrodes so that they do not touch any surrounding muscle tissue and, if needed, cauterize the tissue in contact with the electrodes.
4. Viscoelastic Properties Determination (Lissajous Curves)
- Allow the tongue to rest for 3 - 5 min after the isometric force determination. Perform the Lissajous curves starting at L0, therefore the position of the animal and of the force transducer should never be changed.
- Without stimulating the hypoglossal nerves, apply cycles of passive stretches (Table 2) with increasing displacement (d) i.e. 5, 10, 15, 20, 25, 30, 35, 40, 50% of L0 (higher amplitudes may require a dual mode controller with higher excursion values than the 305C-LR). For example, an amplitude of 40% L0 will cause the deformation of the tongue from +20%L0 to -20%L0.
- Use fixed 2 Hz sine frequency with 10 repetitions in each cycle, for a total duration of 5 s every cycle. Changes of the sine frequency have been used in the past with tissues such as diaphragm24 and could be adopted to modify the experimental protocol.
- Allow 30 s between each cycle and ensure the tongue is wet during the whole procedure.
NOTE: Keep the tongue wet during the procedure adding a few drops of PBS. Ensure that the restraint holding the jaw remains stably in place during the stretches, particularly when the displacement reaches 40% or higher.
- Immediately following the completion of the experiment, while the animal is still under a deep surgical plane of anesthesia, euthanize the animal according to the approved IACUC animal protocol. Dissect the tongue for further processing (i.e. frozen sectioning or storage for biochemical analyses).
Subscription Required. Please recommend JoVE to your librarian.
Representative Results

Figure 3: Representative Results.
(A) Examples of successful twitch and tetanic force traces. The corresponding stimulation is represented by the red trace. (B) Example of unsuccessful tongue tetanic contractions due to submaximal contraction (blue trace) and indirect stimulation of the neck muscles. Both conditions may be improved by repositioning the stimulating electrodes or avoiding the contact between the electrode terminations and the surrounding muscle tissue. (C) Example of sine wave displacement from L0 (25% of L0) used to determine the viscoelastic properties of the tongue. The average lengthening (blue square) and shortening (green square) forces can be used to calculate the Peak-To-Peak force24. The red square indicates the range considered for the analysis (excluding the first and the last sine waves). (D) Representation of the force/displacement relationship as Lissajous loops, obtained increasing the displacement from 5% to 50% L0. The area inside each loop corresponds to the energy loss, defined as the difference between the work done on the muscle to lengthen it and the work done by the muscle as it shortens after the stretch24. Please click here to view a larger version of this figure.
Expected values for twitch and tetanic forces in a 3 month-old Zucker rat (average body weight 400 g for lean and 700 g for obese Zucker rats) are shown in Figure 3A. The tetanic force developed following stimulation should quickly peak (black arrowhead) and then slowly decrease until the stimulation stops. Figure 3B shows examples of unsuccessful contractions in which the force generation did not reach a plateau level before the end of the stimulation (blue line - e.g. if tongue length was set to a value lower than L0, or if the animal's upper body is not entirely stabilized), or in which the stimulus triggered the contraction of the neck muscles (green line). In most of the cases, careful repositioning of the electrodes may improve the contraction. If the neck muscles are visibly contracting during the nerve stimulation, try to isolate any contact point between electrodes and muscle tissue either by cauterizing the muscle or by moving the electrodes away from it. Forces can be normalized by the volume of the tongue measured by MRI if this is available. An alternative to the use of the volumetric data is to normalize against the weight of the tongue after dissection.
An example of Lissajous work loops obtained stretching the tongue from 5% to 50% of L0 is shown in Figures 3C and 3D. Figure 3C shows the length and force traces separately, which when combined as in Figure 3D generate the typical Lissajous loop traces. It is important to ensure that the tongue remains wet between each cycle by adding a few drops of PBS. Increasing displacement from L0 corresponds to higher passive (work done on the muscle during lengthening) and active (work done by the muscle during negative) forces. The analysis of these traces may be complicated. A curve fitting of maximum average force and/or center of mass for each cycle can be used to describe the viscoelastic properties of the tongue. A more detailed analysis of the Lissajous work-loops has been described by D.A. Syme24 using the rat diaphragm.
| Protocol | Pulse Voltage (V) | Pulse frequency (Hz) | Pulse width (ms) | Pulses per train | Train duration (ms) |
| Twitch | 10 | 2500 | 0.2 | 1 | 0.2 |
| Tetanus | 10 | 120 | 0.2 | 96 | 800 |
Table 1: Suggested Contraction Stimulation Parameters.
Isometric twitch contraction is obtained by bilateral nerve stimulation with a single electrical pulse of 10V, lasting 0.2 ms. After 20 s, a tetanic isometric contraction is obtained by stimulating bilaterally with a train of pulses (10 V, 120 Hz frequency, for 800 ms). The twitch/tetanus stimulation is repeated three times with 3 - 5 min interval between each cycle. The highest twitch and highest tetanic forces from the three repetitions are considered for the analysis.
| Total deviation (d) from L0 (%) | Sine amplitude (%L0) | Sine frequency (Hz) | Number of cycles | Time between cycles (s) |
| d | d/2 | 2 | 10 | 30 |
Table 2: Lissajous Curve Parameters (Sinusoidal Deviation from L0).
The application of the Lissajous force/displacement protocol begins 3 - 5 min after the twitch/tetanus stimulation. Each cycle lasts 5 s (10 repetitions at 2 Hz frequency) and is performed 30 s after the previous one. The % displacement from L0 (d) increases at each cycle, from an arbitrary minimum of 5% up to 50% of L0. Higher excursions can be achieved with other force transducer models (Table 3).
Subscription Required. Please recommend JoVE to your librarian.
Discussion
Changes in tongue metabolism and/or composition, e.g. tongue fat infiltration as a consequence of obesity, are predicted to cause quantifiable changes of the parameters assessed by our protocol. The quantification of tongue force is of great interest since an imbalance between protrusive and retrusive activity or overall tongue weakening may result in the occlusion of the upper airway15. Exercise techniques aiming to increase tongue strength have been successfully applied in rats25,26 and also in humans27,28,29, where they effectively decreased the severity of sleep apnea. In addition, hypoglossal nerve stimulation is now a surgical treatment for obstructive sleep apnea22,23,30.
Our experimental protocol aims to guide the user in the analysis of both mechanical and viscoelastic properties of the tongue muscle. The assessment of these parameters has significant translational value, allowing correlation of modern imaging results with functional data. In particular, this technique can be relevant to several fields including speech therapy31, sleep medicine10,25 and the pathogenesis of obstructive sleep apnea15. The described stimulation protocol and parameters can be easily modified to obtain other physiological information such as the force-frequency relationship, fatigability and fatigue recovery capacity, as well as kinetics of muscle contraction in response to stimulation.
When used without the stimulation-evoked force measurements, the passive force/deformation protocol we describe is suitable for repeated analysis over time, since it does not require any of the surgical procedures used for nerve stimulation and force measurements, except for the minimally invasive suturing of the tongue. In this condition, the physiological length of the tongue calculated by MRI can be used as reference (Table 2, parameter d) in place of the measured L0. For this purpose, the use of injectable anesthesia will eliminate the need for tracheal intubation.
A limitation of the current approach resides in the inability to distinguish between protrusive and retrusive components of the tongue contraction. The stimulatory hook electrodes described in this protocol are placed proximal to the bifurcation of the nerve, causing the whole tongue is stimulated to be stimulated. Other groups have described the use of silicon nerve cuff electrodes in rats19,32 or rabbits21, which allow selective access and stimulation of one or both branches of the hypoglossal nerves. Additionally, the use of injectable anesthetics instead of isoflurane inhalation would provide better access to the submandibular region where the hypoglossal nerves branch.
With practice, this protocol is applicable to smaller animals like mice, where the vast majority of disease models are currently available. In particular, a series of mouse models in which tongue physiology is altered are known33,34,35,36. Scaling down will require the utilization of smaller surgical tools, electrodes and tracheal cannulas (if needed), and optionally with a force transducer designed for lower force ranges.
Subscription Required. Please recommend JoVE to your librarian.
Disclosures
The authors have nothing to disclose.
Acknowledgments
This investigation was supported by two National Institutes of Health Grants: HL089447 ("Obesity and OSA: Understanding the Importance of Tongue Fat & Metabolic Function") and HL094307 ("Understanding the Relationship Between Obesity and Tongue Fat")
Materials
| Name | Company | Catalog Number | Comments |
| SurgiSuite (heated Surgical tray) | Kent Scientific | SurgiSuite-LG | Includes heated platform |
| LED Lighting and Magnification Kit | Kent Scientific | SURGI- 5003 | |
| RC2 Rodent Circuit Controller | VetEquip | 922100 | |
| Isoflurane | Butler Schein Animal Health Supply | 29405 | |
| Alcohol Prep | Webcol | 6818 | |
| Cotton-tipped applicators | MediChoice | WOD1002 | |
| Hair clipper | Conair | ||
| Hair remover lotion | Nair | ||
| Medical tape | Transpore | 3M | |
| D-PBS | Corning | 21-030-CM | |
| Operating Scissors | World Precision Instruments | 503717-12 | |
| Hemostatic Forceps | Merit | 97-458 | Any tissue forceps can be used instead |
| Microdissecting Forceps, Angled, Serrated, 10.2 cm, SS | World Precision Instruments | 504479 | |
| Suture Tying Forceps | Fine Science Tools | 18025-10 | |
| Blunt Micro Hook | Fine Science Tools | 10062-12 | |
| Microhemostat | Fine Science Tools | 12075-14 | |
| Thermal cautery | WPI | 501292 | Disposable cauteries are available at lower cost |
| IV 14g x 3.25" cannula | BD | B-D382268H | For tracheal cannulation |
| Braided silk non-absorbable suture size 4-0 | Harvard Apparatus | SP104 | For stabilization of the tracheal cannula |
| Braided non-absorbable silk 5/0 suture | Surgik LC, USA | ESILRC15387550 | For suturing the tongue |
| Plastic-coated metal twist-tie (or electrical wire) | For securing the rat's nose to the platform | ||
| Camera stick | |||
| 3 way-swivel and Trilene 9 Kg test monofilament line | Berkley | For securing the jaw and maintaining the mouth open | |
| Camera stick with adjustable angle | For supporting the 3 way-swivel and maintaining the mouth open. | ||
| in situ Muscle Test System | Aurora Scientific | 809C | This system is designed for mice and was modified by extending the platform. Alternatively the rat-specific 806D system can be used. |
| Dual-Mode Muscle lever (force transducer) | Aurora Scientific | 305C-LR | 309C offers higher excursion capabilities than 305C-LR. Link for more information and specifications: http://aurorascientific.com/products/muscle-physiology/dual-mode-muscle-levers/ |
| Needle Electrodes (surgical steel, 29 gauge) | AD Instruments | MLA1204 | 300C is recommended for use in mice. |
| Magnetic Stands | World Precision Instruments | M10 | Used for making the bipolar stimulating hook electrodes |
| Kite Manual Micromanipulator | World Precision Instruments | KITE-R and KITE-L | Require a steel plate |
| Stackable Double Binding Post with Banana Jack x BNC Jack | McMaster Carr | 6704K13 | |
| Carbon fiber composites digital caliper | VWR | 36934-152 |
References
- Sanders, I., Mu, L. A three-dimensional atlas of human tongue muscles. Anat Rec (Hoboken). 296 (7), 1102-1114 (2013).
- Ciucci, M. R., et al. Tongue force and timing deficits in a rat model of Parkinson disease. Behav Brain Res. 222 (2), 315-320 (2011).
- Easterling, C., Antinoja, J., Cashin, S., Barkhaus, P. E. Changes in tongue pressure, pulmonary function, and salivary flow in patients with amyotrophic lateral sclerosis. Dysphagia. 28 (2), 217-225 (2013).
- Wang, Z. J., Huang, X. S. Images in clinical medicine. Myotonia of the tongue. N Engl J Med. 365 (15), e32 (2011).
- Ota, F., Connor, N. P., Konopacki, R. Alterations in contractile properties of tongue muscles in old rats. Ann Otol Rhinol Laryngol. 114 (10), 799-803 (2005).
- Schwarz, E. C., Thompson, J. M., Connor, N. P., Behan, M. The Effects of Aging on Hypoglossal Motoneurons in Rats. Dysphagia. 24 (1), 40 (2008).
- Pae, E. -K., Wu, J., Nguyen, D., Monti, R., Harper, R. M. Geniohyoid muscle properties and myosin heavy chain composition are altered after short-term intermittent hypoxic exposure. J Appl Physiol. 98 (3), 889-894 (2005).
- Fuller, D. D., Fregosi, R. F. Fatiguing contractions of tongue protrudor and retractor muscles: influence of systemic hypoxia. J Appl Physiol. 88 (6), 2123-2130 (2000).
- Ray, A. D., Farkas, G. A., Pendergast, D. R. In-situ mechanical characteristics of the tongue are not altered in the obese Zucker rat. Sleep. 32 (7), 957 (2009).
- Brennick, M. J., et al. Tongue fat infiltration in obese versus lean Zucker rats. Sleep. 37 (6), 1095-1102 (2014).
- Stedman, H. H., Sweeney, H. L., Shrager, J. B., Maguire, H. C., Panettieri, R. A., Petrof, B., Narusawa, M., Leferovich, J. M., Sladky, J. T., Kelly, A. M. The mdx mouse diaphragm reproduces the degenerative changes of Duchenne muscular dystrophy. Nature. 352 (6335), 536-539 (1991).
- Goodpaster, B. H., Wolf, D. Skeletal muscle lipid accumulation in obesity, insulin resistance, and type 2 diabetes. Pediatr Diabetes. 5 (4), 219-226 (2004).
- Loro, E., et al. IL-15Rα is a determinant of muscle fuel utilization, and its loss protects against obesity. Am J Physiol Regul Integr Comp Physiol. 309 (8), R835-R844 (2015).
- Rahemi, H., Nigam, N., Wakeling, J. M. The effect of intramuscular fat on skeletal muscle mechanics: implications for the elderly and obese. J R Soc Interface. 12 (109), 20150365 (2015).
- Kim, A. M., et al. Tongue fat and its relationship to obstructive sleep apnea. Sleep. 37 (10), 1639-1648 (2014).
- Kim, A. M., et al. Metabolic activity of the tongue in obstructive sleep apnea. A novel application of FDG positron emission tomography imaging. Am J Respir Crit Care Med. 189 (11), 1416-1425 (2014).
- Gilliam, E. E., Goldberg, S. J. Contractile properties of the tongue muscles: effects of hypoglossal nerve and extracellular motoneuron stimulation in rat. J Neurophysiol. 74 (2), 547-555 (1995).
- Sokoloff, A. J. Localization and contractile properties of intrinsic longitudinal motor units of the rat tongue. J Neurophysiol. 84 (2), 827-835 (2000).
- Becker, B. J., Russell, J. A., Connor, N. P. Effects of aging on evoked retrusive tongue actions. Arch Oral Biol. 60 (6), 966-971 (2015).
- Connor, N. P., et al. Tongue muscle plasticity following hypoglossal nerve stimulation in aged rats. Muscle Nerve. 47 (2), 230-240 (2013).
- Seo, J., et al. Nerve cuff electrode using embedded magnets and its application to hypoglossal nerve stimulation. J Neural Eng. 13 (6), 066014 (2016).
- Friedman, M., et al. Targeted hypoglossal nerve stimulation for the treatment of obstructive sleep apnea: Six-month results. Laryngoscope. 126 (11), 2618-2623 (2016).
- Heiser, C., Maurer, J. T., Steffen, A. Functional outcome of tongue motions with selective hypoglossal nerve stimulation in patients with obstructive sleep apnea. Sleep Breath. 20 (2), 553-560 (2016).
- Syme, D. A. Passive viscoelastic work of isolated rat, Rattus norvegicus, diaphragm muscle. J Physiol. 424, 301-315 (1990).
- Connor, N. P., et al. Effect of tongue exercise on protrusive force and muscle fiber area in aging rats. J Speech Lang Hear Res. 52 (3), 732-744 (2009).
- Schaser, A. J., Stang, K., Connor, N. P., Behan, M. The effect of age and tongue exercise on BDNF and TrkB in the hypoglossal nucleus of rats. Behav Brain Res. 226 (1), 235-241 (2012).
- Puhan, M. A., et al. Didgeridoo playing as alternative treatment for obstructive sleep apnea syndrome: randomised controlled trial. BMJ. 332 (7536), 266-270 (2006).
- Guimarães, K. C., Drager, L. F., Genta, P. R., Marcondes, B. F., Lorenzi-Filho, G. Effects of oropharyngeal exercises on patients with moderate obstructive sleep apnea syndrome. Am J Respir Crit Care Med. 179 (10), 962-966 (2009).
- Ueda, H., Almeida, F. R., Chen, H., Lowe, A. A. Effect of 2 jaw exercises on occlusal function in patients with obstructive sleep apnea during oral appliance therapy: a randomized controlled trial. Am J Orthod Dentofacial Orthop. 135 (4), 430 (2009).
- Strollo, P. J., et al. Upper-airway stimulation for obstructive sleep apnea. N Engl J Med. 370 (2), 139-149 (2014).
- Perrier, P., Payan, Y., Zandipour, M., Perkell, J. Influences of tongue biomechanics on speech movements during the production of velar stop consonants: A modeling study. J Acoust Soc Am. 114 (3), 1582-1599 (2003).
- Connor, N. P., et al. Tongue muscle plasticity following hypoglossal nerve stimulation in aged rats. Muscle & nerve. 47 (2), 230-240 (2013).
- Brady, J. P., et al. AlphaB-crystallin in lens development and muscle integrity: a gene knockout approach. Invest Ophthalmol Vis Sci. 42 (12), 2924-2934 (2001).
- Spassov, A., et al. Differential expression of myosin heavy chain isoforms in the masticatory muscles of dystrophin-deficient mice. Eur J Orthod. , ciq113 (2010).
- Lever, T. E., et al. Videofluoroscopic Validation of a Translational Murine Model of Presbyphagia. Dysphagia. 30 (3), 328-342 (2015).
- Gantois, I., et al. Ablation of D1 dopamine receptor-expressing cells generates mice with seizures, dystonia, hyperactivity, and impaired oral behavior. Proc Natl Acad Sci. 104 (10), 4182-4187 (2007).