外围的血管考试
English
Share
Overview
资料来源: 约瑟夫 Donroe,MD、 内科、 儿科,耶鲁大学医学院,纽黑文,康涅狄格
周围血管病 (PVD) 患病率随着年龄的增大和是老年患者,发病的一个重要原因和外周动脉疾病 (PAD) 是伴有心血管和脑血管并发症。糖尿病、 高脂血症、 高血压和烟草的使用是重要的疾病危险因素。当患者出现临床症状时,他们经常抱怨的下肢跛行,定义为恶化与活动,提高了与休息抽筋般的肌肉痛。患者慢性静脉功能不全 (CVI) 经常呈现较低的下肢肿胀、 疼痛、 皮肤变化和溃疡。
筛查无症状的患者为 PVD 好处的虽然不清楚,医生应该知道适当的应试技巧时,正在考虑 PVD 的诊断。这个视频评论上肢和下肢和腹部血管的检查。总是,考官应该使用一种系统的检查方法,虽然在实践中,考试医师执行的程度上取决于他们的底层 PVD 的怀疑。在有或怀疑有血管疾病的风险因素的病人,血管的考试应该是彻底的、 与检验,其次是触诊,和听诊,开始和它应包括特别演习,如确定踝肱指数。同伴视频中演示了利用手持多普勒的演习。
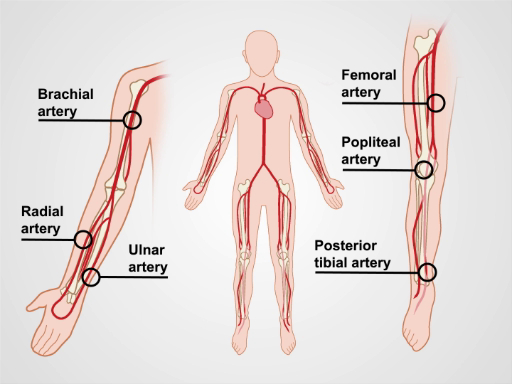
图 1。主要的手臂和腿部动脉。
Procedure
Applications and Summary
Peripheral vascular disease is an important cause of morbidity, particularly in older patients. The detection and subsequent treatment of PVD can improve quality of life and potentially mitigate cardiovascular and cerebrovascular complications. General screening for peripheral vascular disease of the extremities is not a current recommendation by the US Preventive Service Task Force (USPSTF). However, the USPSTF does recommend ultrasound screening for abdominal aortic aneurysms in males who have smoked and are aged 65 to 75. Additionally, the American Heart Association/American College of Cardiology recommends a comprehensive vascular exam in anyone at risk of PVD.
The most important findings that make PAD more likely in a patient include characteristic ulcers, asymmetric temperature difference in the foot, absent pulses, and limb bruits. The most important finding that argues against significant PAD is the presence of at least one pedal pulse on a given leg. A positive Buerger's test increases the likelihood of more extensive disease. Of the physical exam maneuvers to localize the site of reflux in patients with varicose veins, Perthes and Brodie-Trendelenburg tests are the most helpful for ruling out a particular location as the site of reflux. The overall accuracy of these venous reflux maneuvers is limited, however, and detection of the site of reflux is improved through use of a handheld Doppler.
This video reviewed a systematic method and proper technique of vascular examination of the extremities and abdomen, and included a review of special diagnostic maneuvers that should be performed if PVD is suspected. Like all aspects of the physical exam, practice is critical for improving accuracy, and an understanding of the relevant anatomy is important to a successful examination and interpretation of the exam findings.
Transcript
The prevalence of peripheral vascular disease increases with age and it is a significant cause of morbidity in older patients. The peripheral vascular exam plays a key role in bedside diagnosis of this condition.
Peripheral vascular disease, or PVD, includes peripheral artery disease, abbreviated as PAD, and chronic venous insufficiency, or CVI. PAD refers to the narrowing of the peripheral arterial blood vessels primarily caused by the accumulation of fatty plaques, or atherosclerosis. When patients with PAD become symptomatic, they frequently complain of limb claudication defined as a cramp-like muscle pain that worsens with activity and improves with rest. On the other hand, CVI is a condition in which peripheral vein walls become less flexible and dilated, and the one-way valves do not work effectively to prevent the reverse flow. Thus, leading to pooling of blood in the extremities. Patients with CVI often present with lower extremity swelling, pain, skin changes, and ulceration.
When the diagnosis of PVD is being considered, every examiner should follow the proper peripheral vascular exam technique, though the extent of the exam depends on the suspicion of the underlying PVD. This video reviews the general steps for the vascular examination of the upper extremities, the abdomen, and the lower extremities.
Let’s go over the steps involved in a comprehensive peripheral vascular physical examination. Prior to the examination, have the patient put on a gown. This investigation should never occur through clothing. Wash your hands thoroughly before meeting the patient.
Upon entering the room, first introduce yourself and briefly explain the procedure you’re going to conduct. Check the patient’s blood pressure is in both arms. After recording the blood pressure, start with the vascular exam of the upper extremities. Request the patient to lie supine on the exam table with the head raised to a comfortable position. Expose the entirety of both arms and begin with visual inspection. Note symmetry, color, hair pattern, size, skin changes, nail changes, varicosities, muscle wasting, and trauma.
Next, palpate by using the back of the fingers to assess skin temperature. Examine from distal to proximal, comparing one side to the other. Then, assess capillary refill by applying firm pressure over the distal first or second digit for five seconds. Release pressure and count how many seconds it takes for the normal skin color to return. Normal capillary refill time is less than 2 seconds. Following that, palpate for edema over the dorsum of the hands using firm pressure for at least two seconds. If present, palpate proximally, noting the extent and distribution of the edema, and whether or not it is pitting. Grade the edema as trace or mild, which is 1+; moderate or 2+; or severe that is 3+.
Next, palpate the major arteries of the upper extremities. Always use the surface anatomical landmarks to find the pulse. Start by locating the flexor carpi radialis tendon and lateral to that palpate the radial artery. While palpating, note the intensity, rhythm, and symmetry as compared to the other side. Intensity can be described as absent, diminished, normal, or bounding. If unsure, compare the patient’s pulse to your own pulse. Subsequently, locate the flexor carpi ulnaris tendon and slightly lateral to it palpate the ulnar artery. Next, medial to the biceps tendon in the antecubital fossa, palpate the brachial artery. This artery can be followed proximally in the medial groove between the biceps and triceps muscles. For any artery, if no pulse is felt, vary the pressure, and then adjust your position, as there is variability in the path of each artery.
Lastly, if you planning to cannulate the radial artery, perform the Allen’s test. Ask the patient to make a fist and apply sufficient pressure over the ulnar and radial arteries to occlude them. Then instruct the patient to open the fist and note the pallor of the palm. Release the ulnar artery; if sufficient collateral flow is present, the palm should become pink again within 3 to 5 sec. Here we see a sluggish collateral flow, while on the other hand of the collateral flow was good. This concludes the vascular exam of the upper extremities.
Now let’s move to the abdomen. Start by lowering the head of the table so that the patient is lying flat. Adjust the gown to allow sufficient exposure of the abdominal area. First, inspect for dilated veins. If present, follow the procedure described in the text below. Next, locate the abdominal aorta, which is just above the umbilicus and slightly left of the midline. Then, palpate using three to four finger pads of both hands to apply slow and steady downward pressure. The hands should point cephalad and slightly toward each other. Once the pulse is encountered, gradually bring the fingertips closer together until the lateral walls of the aorta are felt. Approximate the distance between the fingers, which is normally less than 3 cm. Following palpation, use the diaphragm of the stethoscope to auscultate the aorta for bruits, while applying moderate pressure. Also, auscultate the renal arteries above the umbilicus and one to two inches lateral to the midline, followed by the iliac arteries below the umbilicus and one to two inches lateral to the midline.
The last part of the vascular exam involves the lower extremities. Begin with inspection, by exposing the entirety of both legs, leaving the genitalia covered. Similar to upper extremities, look for changes in symmetry, color, hair pattern, size, skin changes, nail changes, varicosities, muscle wasting, and trauma. Also, palpate for temperature, perform the capillary refill test, and palpate for the presence of edema. This patient had a non-pitting edema of left leg.
Thereafter, begin with the palpation of the major leg arteries. First, locate the extensor hallucis longus tendon, and palpate the dorsalis pedis artery, which lies just lateral to the tendon. Next, pinpoint the medial malleolus, and posterior and inferior to the malleolus you’ll find the posterior tibialis artery. After that, palpate the popliteal arteries. Place both thumbs on the patellar tendon, slightly flex the patient’s knee and wrap your fingers such that the fingertips land in the middle of the popliteal fossa. If there is difficulty identifying the pulse, gradually flex the knee in 15° intervals while continuing to palpate. If unable to encounter the pulse in this position, have the patient turn to the prone position, flex the knee, and support the lower extremity. Now place your hands on either side of the knee and use the thumbs to palpate the popliteal artery. Next, palpate the femoral arteries, just inferior to the inguinal ligament, approximately midway between the anterior superior iliac spine and the symphysis pubis. Lastly, auscultate the femoral arteries using the bell or diaphragm, while applying light pressure, so as not to artificially induce a bruit.
“This concludes the general peripheral vascular exam. There are other maneuvers that can be done for patients with suspected peripheral vascular disease. However, in reality, these are rarely performed in the office, particularly when imaging is available. These maneuvers include the Buerger’s test for peripheral artery disease. And the Brodie-Trendelenburg test, cough test and the Perthes test for patients with varicose veins. The procedures describing these maneuvers can be found in the accompanying text.”
You’ve just watched JoVE’s video on the peripheral vascular exam. This video reviewed a systematic method and proper technique of vascular examination of the extremities and the abdomen. Like all aspects of the physical exam, practice is critical for improving accuracy of vascular assessment. In addition, an understanding of relevant anatomy is important for correct interpretation of the findings. As always, thanks for watching!
