Source: Suneel Dhand, MD, Attending Physician, Internal Medicine, Beth Israel Deaconess Medical Center
Disorders of the respiratory system with a chief complaint of shortness of breath are among the most common reasons for both outpatient and inpatient evaluation. The most obvious visible clue to a respiratory problem will be whether the patient is displaying any signs of respiratory distress, such as fast respiratory rate and/or cyanosis. In a clinical situation, this will always require emergent attention and oxygen therapy.
Unlike pathology in other body systems, many pulmonary disorders, including chronic obstructive pulmonary disease (COPD), asthma, and pneumonia, can be diagnosed by careful clinical examination alone. This starts with a comprehensive inspection and palpation. Keep in mind that in non-emergency situations the patient's complete history will have been taken already, gaining important insight into exposure histories (e.g., smoking), which could give rise to specific lung diseases. This history can then confirm physical findings as the examination is performed.
Physical Examinations I
Source: Suneel Dhand, MD, Attending Physician, Internal Medicine, Beth Israel Deaconess Medical Center
Learning the proper technique for percussion and auscultation of the respiratory system is vital and comes with practice on real patients. Percussion is a useful skill that is often skipped during everyday clinical practice, but if performed correctly, it can help the physician to identify underlying lung pathology. Auscultation can provide an almost immediate diagnosis for a number of acute pulmonary conditions, including chronic obstructive pulmonary disease (COPD), asthma, pneumonia, and pneumothorax.
The areas for auscultating the lungs correspond to the lung zones. Each lung lobe can be pictured underneath the chest wall during percussion and auscultation (Figure 1). The right lung has three lobes: the superior, middle, and inferior lobes. The left lung has two lobes: the superior and inferior lobes. The superior lobe of the left lung also has a separate projection known as the lingual.
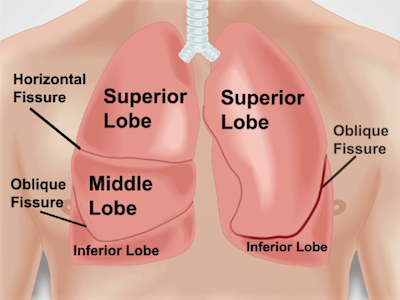
Figure 1. Anatomy of lungs with respect to the chest wall. An approximate projection of lungs and their fissures and lobes to the chest wall anteriorly. RUL - right upper lobe; RML - right middle lobe; RLL - right lower lobe; LUL - left upper lobe; LLL - left lower lobe.
Physical Examinations I
Source: Suneel Dhand, MD, Attending Physician, Internal Medicine, Beth Israel Deaconess Medical Center
The cardiac assessment is one of the core examinations performed by almost every physician whenever encountering a patient. Disorders of the cardiac system are among the most common reasons for hospital admission, with conditions ranging from myocardial infarction to congestive heart failure. Learning a complete and thorough cardiac examination is therefore crucial for any practicing physician.
If there is pathology in the heart or circulatory system, the consequences can also be manifested in other bodily areas, including the lungs, abdomen, and legs. Many physicians instinctively reach straight for their stethoscopes when performing cardiac exams. However, a large amount of information is gained before auscultation by going through the correct sequence of examination, starting with inspection and palpation.
Physical Examinations I
Source: Suneel Dhand, MD, Attending Physician, Internal Medicine, Beth Israel Deaconess Medical Center
Proficiency in the use of a stethoscope to listen to heart sounds and the ability to differentiate between normal and abnormal heart sounds are essential skills for any physician. Correct placement of the stethoscope on the chest corresponds to the sound of cardiac valves closing. The heart has two main sounds: S1 and S2. The first heart sound (S1) occurs as the mitral and tricuspid valves (atrioventricular valves) close after blood enters the ventricles. This represents the start of systole. The second heart sound (S2) occurs when the aortic and pulmonary valves (semilunar valves) close after blood has left the ventricles to enter the systemic and pulmonary circulation systems at the end of systole. Traditionally, the sounds are known as a "lub-dub."
Auscultation of the heart is performed using both diaphragm and bell parts of the stethoscope chest piece. The diaphragm is most commonly used and is best for high-frequency sounds (such as S1 and S2) and murmurs of mitral regurgitation and aortic stenosis. The diaphragm should be pressed firmly against the chest wall. The bell best transmits low-frequency sounds (such as S3 and S4) and the murmur of mitral stenosis. The bell should be applied with a light pressure.
Physical Examinations I
Source: Suneel Dhand, MD, Attending Physician, Internal Medicine, Beth Israel Deaconess Medical Center
Having a fundamental understanding of normal heart sounds is the first step toward distinguishing the normal from the abnormal. Murmurs are sounds that represent turbulent and abnormal blood flow across a heart valve. They are caused either by stenosis (valve area too narrow) or regurgitation (backflow of blood across the valve) and are commonly heard as a "swishing" sound during auscultation. Murmurs are graded from 1 to 6 in intensity (1 being the softest and 6 the loudest) (Figure 1). The most common cardiac murmurs heard are left-sided murmurs of the aortic and mitral valves. Right-sided murmurs of the pulmonary and tricuspid valves are less common. Murmurs are typically heard loudest at the anatomical area that corresponds with the valvular pathology. Frequently, they also radiate to other areas.
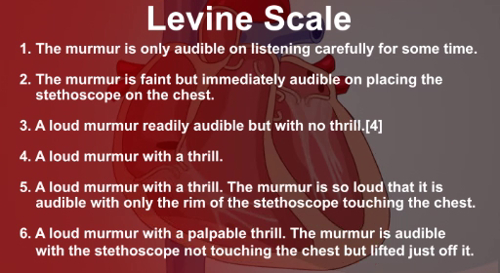
Figure 1. The Levine scale used to grade murmur intensity.
In addition to the two main heart sounds, S1 and S2, which are normally produced by the closing of heart valves, there are two other abnormal heart sounds, known as S3 and S4. These are also known as gallops, because of the "galloping" nature of more than two sounds in a row. S3 is a low-pitched sound heard in early diastole, caused by blood entering the ventricle. S3 is a sign of advanced heart failure, although it can be normal in some younger patients. S4 is heard in late diastole and represents ventricular filling due to atrial contraction in the presence of a stiff ventricle. S4 is also heard in heart failure and left ventricular hypertrophy.
Physical Examinations I
