복부 시험 I: 검사 및 Auscultation
English
Share
Overview
출처: 알렉산더 골드파브, MD, 의학 조교수, 베스 이스라엘 Deaconess 의료 센터, MA
위장병은 매년 수백만 명의 사무실 방문과 입원을 차지합니다. 복부의 신체 검사는 위장관의 질병을 진단하는 데 중요한 도구입니다. 또한 심혈관, 오줌 및 기타 시스템에서 병리학 적 과정을 식별하는 데 도움이 될 수 있습니다. 일반적으로 신체 검사로서, 복부 지역의 검사는 의사-환자 접촉을 확립하고, 예비 진단에 도달하고, 후속 실험실 및 화상 진찰 시험을 선택하고, 배려의 긴급성을 결정하기 위한 중요합니다.
신체 검사의 다른 부분과 마찬가지로, 복부의 육안 검사 및 유도는 잠재적 인 발견을 놓치지 않도록 체계적인 방식으로 수행됩니다. 환자의 역사에 의해 이미 확인된 잠재적인 문제에 특별한 주의를 기울여야 합니다. 여기에서 우리는 환자가 이미 확인되었다는 것을 가정하고, 기록을 취했다, 현상 토론, 및 잠재적인 관심사의 지역이 확인되었습니다. 이 비디오에서 우리는 환자의 역사를 검토하지 않습니다. 대신, 우리는 신체 검사에 직접 갈 것입니다.
시험에 응시하기 전에 복부 부위의 표면 랜드마크, 복부 해부학 및 지형을 간략하게 검토해 보겠습니다. 여기에 유용한 랜드 마크의 목록입니다 : 비용 마진, xiphoid 과정, 정류 복근, 리나 알바, 움빌리쿠스, 일악 문장, 잉구인대, 심칭 음모. 복부 검사는 심포시스 pubis보다 열등하게 시포이드와 비용 마진에서 아래로 영역을 다룹니다.
진단 및 설명 목적을 위해 복부는 오른쪽 위 사분면(종종 RUQ로 지정됨), 왼쪽 상부 사분면(LUQ), 오른쪽 하단 사분면(RLQ), 왼쪽 하부 사분면(LLQ)(그림 1)의네 개의 사분면으로 세분화됩니다. 복부의 더 상세한 지형은 9개의 지역으로 분할합니다: 오른쪽및 좌측 히포콘드리아, 좌우 요추, 좌우 요추, 및 또한 상피위, 탯줄 및 중간위부위(그림 2).
일반적으로 각 복부 부위로 투영되는 장기를 기억하십시오(그림3). 환자의 불만과 증상뿐만 아니라 검사 중 신체적 발견을 적절하게 문서화하고 해석하기 위해 이 지역의 해부학 과 지형을 잘 아는 것이 필수적입니다.
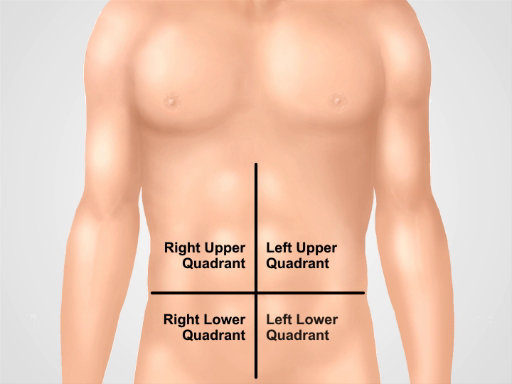
그림 1. 4개의 복부 사분면. 복부는 배빌리쿠스에서 교차하는 두 개의 가상 선으로 나눌 수 있습니다: 오른쪽 상부 사분면(종종 RUQ로 지정), 왼쪽 상부 사분면(LUQ), 오른쪽 하부 사분면(RLQ), 왼쪽 하부 사분면(LLQ)이 표시됩니다.
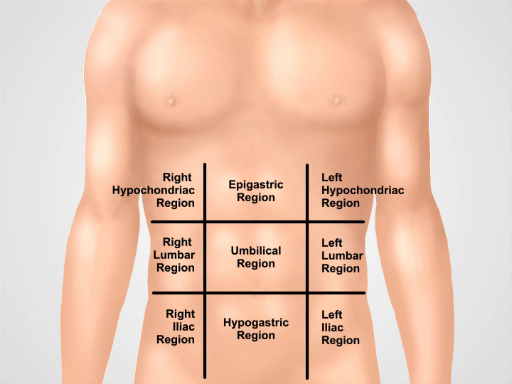
그림 2. 9개의 복부 지역. 중구 선과 하부 및 중구 평면은 복부를 9개의 지역으로 분리합니다: 상복부 지역, 오른쪽 hypochondriac 지역, 좌측 hypochondriac 지역, 탯줄 지역, 오른쪽 요추 지역, 왼쪽 요추 지역, 저위지역, 오른쪽 인기구 지역 및 좌식 인구 부위. 상복부, 배꼽, 저위 및 수부부류 부위에 대한 용어는 임상 실습에서 가장 일반적으로 사용됩니다.
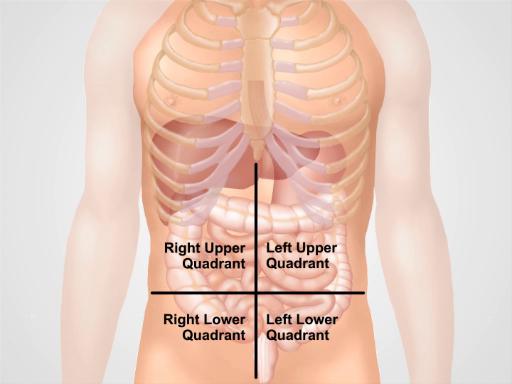
그림 3. 4개의 복부 지구에 있는 다른 기관의 위치. 복강내 의 장기와 4 개의 복부 사분면에 관하여 그들의 위치.
Procedure
Applications and Summary
In this video we reviewed the anatomy of the abdomen and learned how to perform the first two steps of the abdominal examination: inspection and auscultation. Before starting the exam, make sure that the patient is comfortable, well positioned, and adequately draped. Never examine a patient through a gown. Make sure that your hands are washed and warm. Always ask a patient for permission to perform the examination and explain every step of the procedure. Start with a visual inspection of the abdomen. Make note of abdominal contour and symmetry, skin rashes, scars from previous surgeries and injuries, distended veins, and visible peristalses and pulsations. If the presence of ascites, hernias, or masses are suspected, confirm these findings via additional maneuvers that are addressed later on in this video collection.
Omitting visual inspection and/or auscultation steps are common mistakes during an abdominal examination, and can negatively affect a physician’s ability to reach a correct diagnosis. Careful inspection of the abdominal area is especially important. Often times an experienced physician can make a preliminary diagnosis based on a patient’s history and inspection alone. A combination of different pathological signs is of particular diagnostic value. For example, jaundice, ascites, spider angiomas, and caput medusae (distended veins surrounding the umbilicus) can be simultaneously present in a patient with liver cirrhosis.
Once visual inspection is completed, auscultation follows. Auscultate separately for bowel sounds and for bruits. Always perform auscultation before abdominal percussion and palpation. Abdominal auscultation is of clinical significance, especially in a symptomatic patient. The findings should be interpreted in the context of the patient’s history: for example, the absence of bowel sounds in a patient with abdominal pain suggests an abdominal catastrophe (such as peritonitis or the later stages of an intestinal obstruction), but is normal in postoperative patients for a few days following abdominal surgery.
Transcript
Gastrointestinal disease accounts for millions of office visits and hospital admissions annually, which makes the abdominal physical exam one of the most commonly performed assessments. A thorough physical examination not only helps in diagnosing diseases of the gastrointestinal tract, but also aids in identification of pathological processes in cardiovascular, urinary, and other systems. As with the other parts of a physical examination, the assessment of the abdomen also proceeds in a systematic fashion.
This video will begin with a review of the surface landmarks of the abdomen. It will then go on to demonstrate correct patient positioning followed by proper inspection of the abdomen, and precise auscultation techniques. We will also discuss the possible symptoms and their clinical significance.
Before we get to the examination let’s briefly review the surface landmarks of the abdominal region, abdominal anatomy, and topography necessary for interpreting the findings of this exam. The illustration shown here highlights the costal margins, xiphoid process, rectus abdominal muscle, linea alba, umbilicus, ileac crest, inguinal ligament, and symphysis pubis. The abdominal exam covers the area from the xiphoid and costal margins superiorly to the symphysis pubis inferiorly.
For diagnostic and descriptive purposes, the abdomen is subdivided into four quadrants: right and left upper quadrants, and right and left lower quadrants.
The more detailed topography of the abdomen divides it into nine regions: right and left hypochondriac, right and left lumbar, right and left iliac, with epigastric, umbilical, and hypogastric regions in the middle. One should remember which organs typically project into each abdominal region. It is essential to know the region’s anatomy and topography well to adequately document and interpret a patient’s complaints and symptoms, as well as physical findings during the examination.
After taking the history, discussing the symptoms and identifying the potential areas of concern, one can start preparing for the abdominal exam. First step is to ensure that the patient is comfortable and has emptied his or her bladder. Request the patient to lie down supine at about 30-45° angle with the knees slightly flexed. The patient’s arms should be at their side and not folded behind their head, as this tenses the abdominal wall.
Ask the patient for permission to expose their abdominal area… Drape the patient in a way that maintains modesty on one hand, but doesn’t compromise the exam on the other. The abdomen is exposed from above the xiphoid to the suprapubic region. Make sure there is enough light and that noise is minimized. Before approaching the patient wash your hands thoroughly. Then warm your hands and the stethoscope. As with other parts of a physical examination, take a position on the patient’s right side, and explain each step of the exam to them as it progresses.
Start with a visual inspection of the abdomen. Before starting the examination explain to the patient that their abdomen is going to be inspected… Visually inspect the skin looking for rashes, ecchymoses, jaundice, dilated veins, striae, lesions, bruises, and scars. If scars are present, ask the patient about them and document them in the patient’s history.
Examine the shape of the abdomen. Is it flat, protuberant, or scaphoid? Scaphoid abdomen can be seen in cachectic patients, whereas global abdominal protuberance can result from gas, fluid, or fat. Check whether the abdomen looks symmetric or not. Asymmetry is a warning sign and can suggest masses or organomegaly. On the other hand, overall bulging may be sign of fluid accumulation-a condition called ascites. Check for visible hernias and abdominal masses. Pay attention to the presence of visible pulsation or peristalsis, which usually represent a serious problem, for example, abdominal aortic aneurysm. Sometimes visible peristalsis can be seen in intestinal obstruction. Lastly, presence of purplish skin discoloration around the umbilical area indicates a subcutaneous intraperitoneal bleed and is associated with acute hemorrhagic pancreatitis.
Auscultation for abdominal sounds is performed in two or three cycles, each time listening for a particular sound, rather than trying to listen for all the sounds at once.
To begin auscultation, explain the procedure to the patient… After pre-warming the stethoscope, use the diaphragm of the stethoscope to listen for bowel sounds over each of the four abdominal quadrants for 30-40 seconds. Note their frequency and character. Gurgling sounds occurring at a frequency of 5-34 per minute should be heard.
The absence of bowel sounds in an asymptomatic patient shout prompt the physician to listen for longer duration-at least three full minutes-before confirming that the sounds are in fact absent. On the contrary, the absence of bowel sounds in a patient with abdominal pain is a warning sign and might indicate paralytic ileus. Hyperactive, or increased and high-pitched sounds are also abnormal and may be associated with initial stages of bowel obstruction.
Next, listen to different vascular structures at seven different locations, including above the right renal artery, the aorta, the left renal artery, the common iliac arteries, and the femoral arteries for at least five seconds each. While auscultating these arteries, one should listen for bruits, which are the audible vascular “swishing” sounds caused by turbulent flow in large arteries. Their presence can indicate stenosis in renal, iliac and femoral arteries, or suggest abdominal aortic aneurism. Finally, listen for friction rubs over the liver and spleen. This is a rare finding that suggests inflammation of the peritoneal surface of the organ from infection, tumor, or infarct.
You’ve just watched JoVE’s presentation on the first two parts of the physical abdominal examination. Now you should have a good understanding of the surface landmarks of the abdomen and know how to conduct the inspection and auscultation steps of this exam. The following two videos will discuss: abdominal percussion, and light and deep palpation steps of abdominal assessment. As always, thanks for watching!
