남성 직장 시험
English
Share
Overview
출처: 조셉 돈로, MD, 내과 및 소아과, 예일 의과 대학, 뉴 헤이븐, CT
암 검열에 있는 그것의 유용성은 토론되는 동안, 남성 직장 검사는 신체 검사의 중요한 부분으로 남아 있습니다. 시험은 더 낮은 요로 현상, 요로 및/또는 대변 요실금 또는 보존, 요통, 상영 증상, 복부 불만, 외상 환자, 설명할 수 없는 빈혈, 체중 감소 또는 뼈 통증을 가진 선택된 환자에서 표시됩니다. 직장 시험에는 절대적인 금기 사항이 없습니다. 그러나, 상대적인 금기에는 시험을 거치려는 환자 의지, 심한 직장 통증, 최근 상향 수술 또는 외상 및 호중구 감소증이 포함됩니다.
직장 검사를 수행할 때 심사관은 관련 해부학을 개념화해야 합니다. 외부 항문 괄약근은 항문 운하의 가장 단산 부분이며, 이는 직장으로 전환하기 전에 3 ~ 4 센티미터를 확장합니다. 전립선선은 항문 운하 바로 너머의 직장에 앞쪽으로 놓여 있습니다. 전립선의 후방 표면은 정점, 염기, 측면 엽 및 중앙분리대를 포함하여 직장 벽을 통해 만져질 수있다(도 1). 전립선의 정상적인 일관성은 손이 꽉 주먹에있을 때 테나 명성과 유사합니다. 엄지 손가락 너클은 딱딱한 멍청이가 어떤 느낌일지 대표합니다. 전립선의 정상적인 크기는 나이에 따라 증가하고 젊은 남자에서 약 4.0 cm x 3.5 cm, 또는 20-30 g입니다.
준비, 포지셔닝, 신경학적 평가, 외부 검사 및 심포팅, 전립선 및 직장 검사, 대변 평가 등 남성 직장 검사의 단계는 이 동영상에 자세히 설명되어 있습니다.
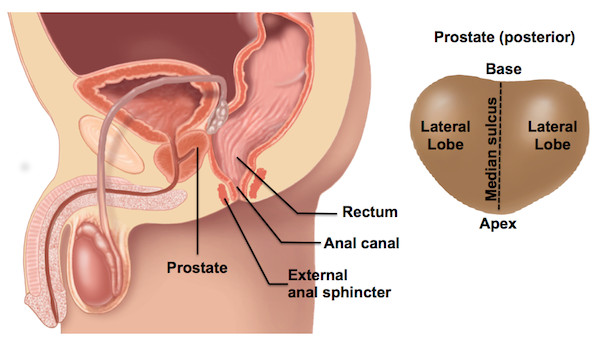
그림 1. 남성 직장 해부학 (왼쪽) 및 전립선 후방 표면의 영역 (오른쪽).
Procedure
Applications and Summary
The male rectal exam remains an important part of the physical exam, particularly for patients with abdominal, genitourinary, or gastrointestinal concerns. It is a sensitive procedure and requires careful attention to verbal and body language to ensure patient comfort. This video reviewed the indications and contraindications for the exam, relevant anatomy, as well the steps involved in performing the examination. Abnormalities that may be encountered at each step are found in Table 1. Physician comfort and technical proficiency with the rectal exam improves through practice, and the accuracy of the exam correlates with the experience of the examiner. As in other aspects of the physical exam, it is important to have a systematic method of examination. The method demonstrated in this video involves neurologic assessment, inspection and palpation of the perianal region, palpation of the prostate, palpation of the rectum, and finally, inspection of any stool on the gloved finger after the exam.

Table 1. Abnormalities detected during the male rectal exam. The table shows potential pathological findings that can be observed during rectal examination and their interpretations.
Limitations of the rectal exam are important to become familiar with. The rectum extends 12 to 15 cm beyond the anal canal, thus only the most distal portion can be palpated. Additionally, determining prostate size by DRE may be unreliable and thus should be considered an approximation. When compared with experienced urologists, students tend to palpate fewer areas of the prostate and use insufficient pressure, both of which limit detection of nodules. The examiner should always attempt to palpate the prostate from apex to base and both lateral lobes. However, with larger prostates, the examiner's finger may not be long enough to reach the base, limiting the evaluation. Finally, early malignancy is unlikely to be detected by DRE alone, thus screening for prostate cancer should be done with concomitant prostate specific antigen (PSA) testing in the appropriate patients.
Transcript
The male rectal exam remains an important part of the physical exam, particularly for patients with abdominal, genitourinary, or gastrointestinal concerns. Being a sensitive examination, it is extremely important that a physician knows how to conduct the steps in an appropriate manner, such that the patient’s modesty is maintained without compromising the outcome of the exam.
Clinical indications for this exam include: lower urinary tract symptoms, urinary incontinence or retention, fecal incontinence or retention, back pain, anorectal symptoms, abdominal complaints, trauma patients, unexplained anemia, weight loss, or bone pain. This video will review the relevant anatomy of the male rectal area. And then it will provide the steps needed to conduct a comprehensive examination in a sensitive yet effective manner.
When performing the rectal exam, the examiner should conceptualize the relevant anatomy. The external anal sphincter is the most distal part of the anal canal. This canal is approximately three to four centimeters long and just beyond it lays the rectum, and anterior to the rectum is the prostate gland.
This gland is approximately 4 cm by 3.5 cm and 20-30 grams in a young man. Although its size normally increases with age. The posterior surface of the prostate, including its apex, base, median sulcus and lateral lobes, can be palpated through the rectal wall. The normal consistency of the prostate is similar to the thenar eminence when the hand is in a tight fist. The thumb knuckle is representative of what a hard nodule may feel like.
Now that we have reviewed the anatomy, let’s discuss the essential steps of the examination. Inform the patient of the exam about to be performed and the reason for it. Recognize that some men may feel uncomfortable at the idea of having the exam performed. If it seems a patient feels uncomfortable with the exam, take a moment to explore the reasons why. Discussing the exam in a matter of fact way tends to lessen a patient’s anxiety. As with all sensitive examinations, it is important to be mindful of the language used during the exam. While conducting the exam, tell the patient what you intend to do before actually performing the maneuver. In general, avoid words that can have intimate connotation, such as “feel”, “touch”, and “looks good”, as well as words that are overly medical, such as “probe” and “palpate”. Some useful neutral words include “examine”, “check”, “assess”, “insert”, and “appears healthy”.
Before beginning the exam, be sure everything needed is ready in advance. Prepare one pair of latex-free gloves, lubricant pre-expressed on a paper towel, a cotton swab for neurologic examination, tissue paper for patient to clean self after the exam, and guaiac card and reagent-if testing for occult blood. Once the patient is comfortable, wash your hands and put on your latex-free gloves. Then, apply a thin layer of lubricant to your dominant index finger; be sure to apply enough lubricant to cover the entire length and circumference of the finger. Applying too much leads to an unnecessary mess, while applying too little causes patient discomfort.
Next, position the patient. There are three acceptable ways to position a patient for the rectal exam: the Sims’ position, the modified lithotomy position and the standing position. For the Sim’s position, have the individual lie down on the examination table. Then, instruct the patient to roll onto his left side with his left leg straight and right leg flexed at the hip and knee to 90°. Alternatively, both legs can be flexed at hips and knees to 90°. For modified lithotomy position, have the individual lie on his back with his feet together and hips and knees bent. For the third position, direct the patient to stand in front of the exam table with feet shoulder-width apart. Have the patient bend forward at the waist and support himself on his elbows and forearms. Throughout the procedure, expose only the area necessary to perform a thorough exam, and then cover the patient as soon as the examination of that body part is completed. Also, be careful to avoid unnecessary physical contact, including the inadvertent contact between your leg and the patient.
Begin by carefully inspecting the skin of the patient’s buttocks, sacrococcygeal and perianal regions. Look for any ulcers, drainage, masses or nodules. You may use your hands to separate the buttocks, or you may ask the patient to reach back with his right hand and pull his right buttock forward. Be sure to carefully palpate any abnormal areas identified during your perianal inspection. In patients with neurologic symptoms or lower back pain, perform the neurological assessment of the perianal sensation. Using a cotton swab, gently touch the patient’s perianal region in a dermatomal pattern. Ask the patient to notify you when you contact his skin.
Next, test the patient’s anal reflex by using the cotton swab to gently scratch the skin surrounding the anus. Observe the sphincter for contraction. Following neurologic assessment, you should perform the digital rectal examination, which is mainly done to examine the prostate and the rectum. Inform the patient that he may feel the urge to have a bowel movement. And reassure that this is normal and an actual bowel movement will not occur.
First, ask your patient to bear or strain down, as if he was having a bowel movement. Next, with gentle pressure, place your lubricated fingertip on your patient’s external anal sphincter, and pause. If the patient experiences pain or the sphincter tightens, then wait for a moment. Once you feel the sphincter relax, then fully insert your finger. Note the patient’s sphincter tone during insertion. Ask the patient to squeeze down on your finger if the clinical context calls for a complete neurologic exam.
Next, palpate the posterior surface of the prostate through the patient’s rectal wall. The prostate can be encountered by directing your finger anteriorly toward the umbilicus. Then locate the median sulcus, which runs between the lateral lobes of the prostate. Follow it until the base of the prostate is felt. This may be beyond the length of your finger. Examine each lateral lobe of the prostate using abduction, adduction, flexion, extension, supination and pronation movements of your finger. Use sufficient finger pressure to enhance detection of smaller lesions. Be sure to note the relative symmetry of size, consistency, areas of nodularity and tenderness. Use your fingertip to approximate the size of the prostate. Each fingertip-sized area is approximately 10-15 grams. Lastly, with your finger fully inserted, proceed to palpate the rectum. Begin by rotating your hand clockwise from six o’clock to one o’clock, and then back to the 6 o’clock position. Then, rotate your hand counter-clockwise to twelve o’clock by turning your body away from the patient.
Once complete, withdraw your finger smoothly and replace the gown to avoid exposing the patient for longer than necessary. Hand the patient tissue paper and invite him to clean himself. If a curtain is available, close it at this point to allow for privacy. Inspect any stool that may be on your gloved hand for color, consistency and blood. If necessary, use the guaiac card to test for occult blood. Then, carefully dispose of your gloves and wash your hands thoroughly. Once the patient is ready, review any normal and abnormal findings with him and discuss the subsequent steps to be taken, if necessary.
You have just watched a JoVE video documenting the male rectal examination. You should now understand the systematic sequence of steps every physician should follow in order to conduct an effective male rectal examination in a sensitive manner. As always, thanks for watching!
