呼吸試験 II: 打診と聴診
English
Share
Overview
ソース: Suneel Dhand、MD、医師、内科、ベス イスラエス ディーコネス メディカル センターに参加
打楽器と呼吸器系の聴診のため適切な技術を学習が重要であると、実際の患者に実際に付属しています。パーカッションは毎日の臨床実習中にスキップはしばしば有用なスキルが、基になる肺の病理を識別するために医師を助けることができる場合は、正しく実行します。聴診は、急性の肺等の慢性閉塞性肺疾患 (COPD)、喘息、肺炎、気胸の数にほぼ即時診断を提供できます。
肺の聴診のエリアは、肺のゾーンに対応します。打診と聴診(図 1中に胸壁下に各肺葉を描写できます)。右肺は 3 葉: 優れた, 中, と下葉。左肺は 2 つの葉: 優れたと劣る葉。左肺の上葉舌として知られている別の投影があります。
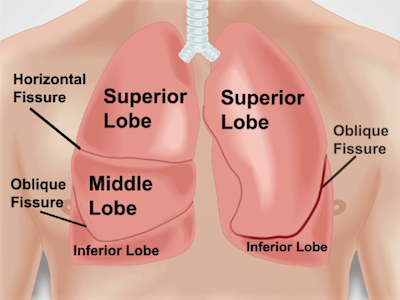
図 1。胸壁に対して肺の解剖学.肺の近似射影亀裂と胸に葉の前方壁します。時代 – 右上葉;RML – 右肺中葉。RLL – 右下葉;LUL – 左上葉;LLL – 下葉を左します。
Procedure
Applications and Summary
Percussion and auscultation should always be done in sequence whenever performing a full respiratory examination. Learning how to percuss correctly takes time and practice (practice can be done on yourself or other surfaces, such as a table). Note how the percussion note changes naturally over air-filled lung, ribs, and solid organs, such as the heart.
Auscultation must be performed over each lung zone to give the physician the best chance of identifying the focus of any lung pathology. Abnormal breath sounds should be easily recognizable when occurring in a patient. Allow enough time to classify the breath sounds. Listen for several breathing cycles in one area, if necessary, to hear the exact nature of the crackles, wheezes, rhonchi, or other pathological findings. Distinguishing between certain breath sounds can occasionally seem subjective, but will become easier with practice, leading to a "spot diagnosis" for many pulmonary conditions.
Transcript
Learning the proper technique for percussion and auscultation of the respiratory system is vital for the bedside diagnosis of lung disorders. Percussion is a simple yet useful skill, which, if performed correctly, can help the physician identify the underlying lung pathology. On the other hand, auscultation can provide an almost immediate diagnosis for a number of pulmonary conditions including chronic obstructive pulmonary disease, asthma, pneumonia, and pneumothorax.
In another video, we covered how to perform inspection and palpation of the respiratory system. This video will focus on the percussion and auscultation steps of this exam.
Before going into the details of the clinical exam, let’s review the lung lobes and breath sounds. This will help us better understand the anatomical locations and results of percussion and auscultation.
The areas for percussion and auscultation of lungs correspond to the lung lobes and each lung lobe can be pictured underneath the chest wall. The right lung, which is the larger of the two, has three lobes-superior, middle, and inferior. The horizontal fissure separates the superior from the middle lobe, whereas the right oblique fissure separates the middle from the inferior. The left lung only has two lobes- superior and inferior-separated by the left oblique fissure. Since lungs are mostly filled with air that we breathe in, percussion performed over most of the lung area produces a resonant sound, which is a low pitched, hollow sound. Therefore, any dullness or hyper-resonance is indicative of lung pathology, such as pleural effusion or pneumothorax, respectively.
Breath sounds heard through the stethoscope during auscultation are peculiar as well. The two sounds heard during normal breathing are bronchial and vesicular. Bronchial sound, which is more tubular and hollow, is heard over the large airways in the anterior chest. Whereas, vesicular sound, which is soft, low-pitched and rustling, can be heard over most of the lung tissue area. Abnormal breath sounds include crackles also known as rales,which are indicative of fluid in small airways. On the other hand, wheezes or rhonchi suggest airway constriction or swelling, which causes partial airway obstruction. Pleural rubs occur when inflamed pleural surfaces slide against one another during respiration, and lastly stridor is caused by obstruction of the upper airway.
With this knowledge of where and what to look for during respiratory percussion and auscultation, let’s discuss the procedural steps starting with percussion. Ask the patient to sit straight or lean forward. Start with the percussion of the posterior surface. Place your non-dominant hand with middle finger pressed and hyperextended firmly over the patient’s mid-back area. Use the tip of the middle finger of the dominant hand to tap firmly on the top third phalanx of the middle finger of the pressing hand at least twice. Repeat this at four to five levels, comparing side-to-side.
Perform the same procedure on the anterior chest wall, working from the inferior lung borders. Both anteriorly and posteriorly, make sure the middle finger of the pressing hand is placed in the intercostal spaces and not on the ribs. Appreciate the percussion sound quality. Tapping over normal air-filled lung should produce a resonant percussion note. On the contrary percussion over solid tissues such as the liver or the heart should produce a dull note. And percussion over hollow spaces, like the Traube’s space should yield a Tympanic note, which is a drum-like sound.
Lastly, let’s move to auscultation, which is listening to breath sounds using a stethoscope. To start, instruct the patient to lean forward or sit upright in order to examine posteriorly. Request the patient to place their hands on opposing shoulders to get maximum exposure to the lung fields. Place the diaphragm on the patient’s mid-back area and ask them to take deep breaths in and out through their mouth. Auscultate at five levels posteriorly, and then repeat the same procedure anteriorly, comparing side-to-side. Normal breath sounds should be symmetrical both posteriorly and anteriorly; any deviation is a possible indicator of a lung disease.
The last three steps of auscultation are tests aiming to identify lung consolidation. First of these tests is to assess for bronchophony. Ask the patient to say “99”, while auscultating the chest area. An increased sound transmission indicates a consolidated lung. Second is to assess for egophony. Ask the patient to say “E”. When an “E” sound changes to an “A” through the stethoscope, it is an indication of a consolidated lung. Lastly, assess for whispering pectoriloquy. Ask the patient to whisper “99”. In case of a consolidated lung, the sound will actually be heard better and more clearly through the stethoscope. All these steps should also be performed posteriorly at different locations in order to cover the entire lung area. At the end of the examination, thank the patient and have them change back.
You’ve just watched JoVE’s video on percussion and auscultation for respiratory evaluation. Distinguishing between sounds heard during this portion of the exam can occasionally seem subjective, but the assessment becomes clearer and easier with practice, leading to a “spot diagnosis” for many pulmonary conditions. As always, thanks for watching!
