Enucleation of the Prostate for the Treatment of Benign Prostatic Hyperplasia Using a 980 nm Diode Laser
Summary
Here, we present a protocol for modified 980 nm diode laser enucleation to treat large volume benign prostatic hyperplasia.
Abstract
In the aging male population, the occurrence of lower urinary tract symptoms (LUTS) caused by benign prostatic hyperplasia (BPH) is a common problem. Here, we introduce a new technique called 980 nm diode laser enucleation (DiLEP) to treat BPH1. Diode lasers can absorb both water and hemoglobin at the same time, so they are good for cutting and hemostasis2. The diode laser was approved by the FDA in 2007, and has been used in the treatment of BPH because of its effective cutting and hemostasis effect3. DiLEP presents several advantages over other techniques, such as TURP, HoLEP, and PVP. During the procedure, we define the boundary of a high-volume prostate and separate it into three lobes with a diode laser by burning two rings and one groove (like a Cupid's arrow). Compared to other procedures, mDiLEP has fewer intraoperative complications, a shorter learning curve, and achieves more tissue resection.
Introduction
Compared with traditional transurethral resection of the prostate (TURP), laser surgeries have gradually become more popular due to their better patient tolerance, lower amounts of intraoperative blood loss, efficacy, and shorter postoperative recovery4,5.
In recent years, the fastest growing techniques have involved the use of lasers of various wavelengths. At present, many types of lasers with different characteristics can be used to complete prostate enucleation. Since the diode laser was approved by the US FDA for prostatic hyperplasia in 2007, its use has gradually increased in the treatment of BPH because of its outstanding cutting ability and hemostasis effect6. The laser wavelength determines the degree of absorption by water and hemoglobin. A diode laser with a wavelength of 980 nm provides the highest combined absorption rate of water and hemoglobin. The tissue penetration ability is 0.5 mm, and it can produce coagulation effects in deeper tissue, which makes it have a very good tissue ablation and hemostasis ability7,8.
Many research centers have begun to use DiLEP for the treatment of benign prostatic hyperplasia. In practice, traditional DiLEP has a longer learning curve and presents no obvious advantages related to urinary sphincter protection9. Based on the above reasons, traditional DiLEP was modified in our center to improve the value of diode laser treatment in patients with BPH.
Protocol
All methods described here have been approved by ethics committee of Beijing Hospital. Indications for surgery are according to the European Association of Urology guidelines for nonneurogenic male LUTS. Contraindications include suspected prostate cancer or detrusor dysfunction.
1. Instruments for operation
- Ensure the availability of diode laser (980 nm) equipment with a power including continuous mode (80-100 W).
- Employ a laser fiber and 0.9% saline solution for intraoperative bladder irrigation.
- Use a 26 F laser resectoscope to acquire good visualization and enhance efficiency.
2. Preparation for operation
- Perform skin preparation on the day of the operation.
- Provide an intravenous antibiotic preoperatively to all patients10.
NOTE: Cefuroxime sodium (1.5 g in 100 mL of 0.9% sodium chloride) is provided 30 min before the operation. - Before anesthesia, make the patient lay down on the operating table.
NOTE: General anesthesia is effective and appropriate for this operation. The anesthetists should determine the mode of anesthesia depending on the patient's general condition. - Drape the patient in a sterile fashion in the dorsal lithotomy position.
3. Procedure steps
- Observation
- Directly observe the urethra, verumontanum, bladder neck, ureteral orifices, bladder mucosa, and trabecular hyperplasia by resectoscope (15-30°).
- Design the range of enucleation (Cupid's arrow).
- Circularly incise (depth to gland, width about 3-4 mm) the bladder neck mucosa with a laser (Figure 1).
- Circularly incise (depth to gland, width about 3-4 mm) the prostatic urethra mucosa at the proximal end of the verumontanum with a laser (Figure 2).
NOTE: Confirm anatomical mark before incision in order to avoid injury of the bladder neck mucosa and sphincter urethrae. Use a laser power of 80-100 W during the operation except for hemostasis. - Connect the concentric circles of the bladder neck and the apex of the prostate in the posterior urethra at a 12 o'clock position.
- Incise the left lobe and right lobe with the laser (Figure 3).
NOTE: Once the 12 o'clock position of the posterior urethra is pre-incised, retain the distal mucosa. The concentric circles formed at the neck of the bladder and the apex of the prostate are called Cupid's arrows.
- Making a channel
- Find the surgical capsule at the 5 and 7 o'clock positions of the apex of the prostate.
- Find the surgical capsule at the 5 and 7 o'clock surgical capsule positions.
- Connect the 5 and 7 o'clock surgical capsule positions with a laser (Figure 4).
- At the 6 o'clock position of the apex of the prostate, separate the median lobe from the surgical capsule from the apex of the prostate to the bladder neck with a laser (Figure 5).
NOTE: If the volume of the prostate is >80 mL, the median and lateral lobes will be completely separated at the 5 and 7 o'clock positions of the apex of the prostate.
- Enucleation of the left and right lobes
- In a counterclockwise direction, enucleate the right lobe at 6 and 12 o'clock from the apex of the prostate to the bladder neck with a resectoscope (Figure 6).
- In a clockwise direction, enucleate the left lobe at 6 and 12 o'clock from the apex of the prostate to the bladder neck (Figure 7).
- Push all the glands into the bladder after enucleation.
NOTE: If the volume of the prostate is >80 mL, enucleate the median and lateral lobes in the proper sequence; then, push into the bladder.
- Hemostasis
- Use a lower laser power (50 W) to stop bleeding around the surgical site. Maintain an appropriate distance (i.e., 1-3 mm).
- Morcellate the prostate tissue.
- Morcellate the enucleated prostatic tissue into small pieces (as small as possible) with a morcellator and then remove the tissue from the bladder (Figure 8).
- Catheterization
- Remove the morcellator from the urethra.
- Gently place a 22 F Foley catheter through the urethral orifice into the bladder cavity with 30 mL of water in the balloon after sufficiently lubricating the urethra with lidocaine gel.
- Postoperative care10
- Let the patient lay down on the bed for approximately 3 h postoperatively in the care unit until they completely wake up from anesthesia. Make sure that patient monitors and medical oxygen are available during this time.
- Once the patient has completely woken up, return the patient to the ward. Let the patient begin to drink some water and eat some food. Record any urine output and pay attention to the color of the urine.
Representative Results
A total of 40 patients with BPH who underwent DiLEP were included in one of our studies. An independent sample t-test was used as the statistical method. All patients successfully completed the operation. Almost all of the patients had the catheter removed within 5 days postoperative (Table 1). All patients returned to the hospital for follow-up examinations in the 1st, 3rd, and 12th months postoperatively. The International Prostate Symptom Score (IPSS)11 and Quality of Life (QoL)1 tools were used to screen for, rapidly diagnose, track the symptoms of, and guide the management of BPH. These can also be used to evaluate the efficacy of the BPH treatment. Compared to the baseline values, the International Prostate Symptom Score (IPSS) significantly decreased to 38.15%, 31.92%, and 18.70% at 1, 3, and 12 months postoperatively, respectively (all p < 0.001), and the QoL significantly decreased to 57.89%, 43.94%, and 20.78% (all p < 0.001, respectively). For objective parameters, compared to the baseline, the mean Qmax increased nearly 3x, and the mean postvoid residual during follow-up decreased nearly 4x. Compared to the preoperative values, postoperatively, the prostate volume decreased dramatically (p < 0.001) (Table 2).
The peri- and postoperative complications reported during this study are presented in Table 3. According to the modified Clavien Dindo classification system12, a widely used and authoritative tool for grading surgical complications, no intraoperative patient had complications, and only four cases reported Grade 1 postoperative complications12.

Figure 1: Circularly incise the bladder neck mucosa with a laser. Please click here to view a larger version of this figure.

Figure 2: Circularly incise the prostatic urethra mucosa at the proximal end of verumontanum with a laser. Please click here to view a larger version of this figure.

Figure 3: Incise the left lobe and right lobe at the apex of the prostate at 12 o'clock. Please click here to view a larger version of this figure.

Figure 4: Circularly incise the bladder neck mucosa with a laser. Please click here to view a larger version of this figure.

Figure 5: Find the surgical capsule at the 5 and 7 o'clock positions of the apex of the prostate and connect the 5 and 7 o'clock surgical capsule positions with a laser. Please click here to view a larger version of this figure.

Figure 6: In a counterclockwise direction, enucleate the right lobe at the 6 and 12 o'clock positions from the apex of the prostate to the bladder neck. Please click here to view a larger version of this figure.

Figure 7: In a clockwise direction, enucleate the left lobe at the 6 and 12 o'clock positions from the apex of the prostate to the bladder neck. Please click here to view a larger version of this figure.
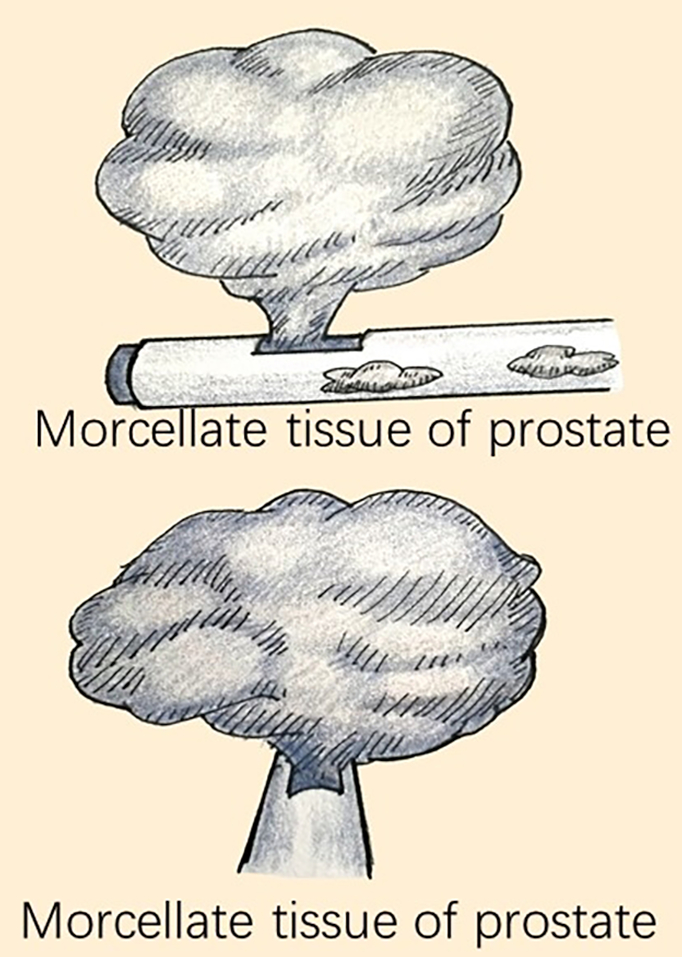
Figure 8: Cut the enucleated prostatic tissue into small pieces using a morcellator and then remove the tissues from the bladder. Please click here to view a larger version of this figure.
| Parameters | Data |
| Age (y) | 73.35±7.84 |
| Prostate volume (ml) | 106.40±19.01 |
| Operative time (min) | 71.18±16.55 |
| Perfusion fluid volume (L) | 28.02±13.80 |
| Postoperative irrigation time (h) | 13.47±1.83 |
| Decrease in hemoglobin (g/L) | 2.62±1.24 |
| Catheter duration (d) | 4.25±0.08 |
| Hospital stay (d) | 4.60±0.77 |
| Follow-up time(m) | 12.45±1.75 |
| Data are shown as mean ± SD;BPH: Benign prostatic hyperplasia; diode laser enucleation of the prostate; SD: Standard deviation | |
Table 1: Perioperative data of 40 patients with BPH who underwent DiLEP.
| Parameters | Pre-operative | 1m | 3m | 12m | P-value |
| Qmax (ml/min) | 7.12±2.94 α,β,γ | 21.19±2.18 | 22.24±2.02 | 19.73±1.80 | <0.001 |
| PVR(ml) | 113.22±33.56 α,β,γ | 27.30±3.98 | 25.05±4.21 | 31.10±6.65 | <0.001 |
| IPSS | 23.15±7.44 α,β,γ | 8.37±2.49 | 7.37±1.94 | 4.33±1.79 | <0.001 |
| QOL | 3.80±0.88 α,β,γ | 2.20±0.89 | 1.67±0.65 | 0.79±0.66 | <0.001 |
| PV(ml) | 106.40±19.01 | —— | —— | 22.08±4.28 | <0.001 |
| Qmax = maximum flow rate; PVR = postvoid residual; IPSS = International Prostate Symptom Score; QoL = quality of life; PV = prostate volume | |||||
| α:Significant differences between pre- and post-operative 1 month groups; β:Significant differences between pre- and post-operative 3 months groups; γ:Significant differences between pre- and post-operative 12 month |
|||||
Table 2: Data at baseline and at 1, 3, and 12 months postoperatively parameters.
| Complications | Patients, n (%) | Grade |
| Intraoperative | ||
| Prostate capsule perforation | 0 | 3b |
| Blood transfusion | 0 | 2 |
| TURP syndrome | 0 | 4 |
| Bladder wall injury | 0 | 2 |
| Ureteric orifce injury | 0 | 2 |
| Urethra sphincter injury | 0 | 2 |
| Postoperative | ||
| Bladder convulsion | 2 (5%) | 1 |
| Urge urinary incontinence | 2 (5%) | 1 |
| Stress urinary incontinence | 0 | 2 |
| Re-place the catheter | 0 | 1 |
| Complications were graded according to the modifed Clavien-Dindo classifcation system | ||
Table 3: Peri- and post-operative complications of 40 patients with BPH who underwent DiLEP.
Discussion
At present, the 980-mm diode laser is beginning to be used for the treatment of BPH5. Few reports have described related clinical studies. Compared to the effect of TURP in the treatment of BPH, many studies have shown that DiLEP causes less blood loss, achieves better urination function, and has shorter catheter retention times9,13,14,15.
Here, we share our experiences with mDiLEP. In our study, compared with traditional DiLEP9,16,17, we circularly incised the bladder neck mucosa and the prostatic urethra mucosa at the proximal end of the verumontanum with a laser before enucleation. Then, we connected the concentric circles of the bladder neck and the apex of the prostate at 12 o'clock. This is called a Cupid's arrow. Although this procedure seemed to increase the operation time, it did not increase the total operation time relative to results described in other studies. It also brings many benefits: First, the urethral sphincter is protected from injury because we circularly incised the prostatic urethra mucosa at the proximal end of the verumontanum18. The preserved urethral mucosa at the apex of the prostate can function like an anal cushion, allowing the urethral sphincter to work better, improving the prevention of urine leakage. For the above reasons, no patient reported stress urinary incontinence in this study. Second, surgeons can operate within a delimited surgical area by circularly incising the bladder neck mucosa with a laser, which can protect ureteral orifices from injury. These two steps are not performed in traditional operations. Some studies11,19,20 have reported that the incidences of urethral sphincter and ureteral orifice injuries are relatively high, especially for inexperienced surgeons, and the occurrence of these complications is a heavy burden for doctors and patients. Third, the operator can define the scope of surgery by incising the bladder neck mucosa and the prostatic urethra mucosa at the proximal end of the verumontanum. This helps the surgeon find the prostate surgical capsule, reduces the occurrence of prostate capsule perforation, and facilitates the enucleation of the median and lateral lobes21. According to our experience, this operation involving a Cupid's Arrow was much easier to master and facilitates the promotion of this new technology.
Compared to existing procedures used in BPH treatment, DiLEP demonstrates satisfactory short-term clinical outcomes. In addition, this promising technique has obvious advantages in that it prevents urinary continence. However, more research is needed to demonstrate the long-term efficacy of this technique. Only in this way can this technique be developed into a blueprint for a prostate enucleation protocol in the future.
Disclosures
The authors have nothing to disclose.
Acknowledgements
The authors would like to acknowledge the support of the National Key Research and Development Program of China (Grant 2017YFC840102).
Materials
| HU Diode Laser | Beijing L.H.H.Medical Science Development Co., Ltd | HU-150 | Wavelength: 980nm Maximum Power: 150W Operation Mode: Continuous and pulsed |
| Optical Fiber | Beijing L.H.H.Medical Science Development Co., Ltd | YYGX600 | Fiber core diameter: 600 μm Fiber length: 2m |
| Morcellator System | Beijing L.H.H.Medical Science Development Co., Ltd | PXQ-01 | Rotate Speed: 100-3000rpm MAX. Vacuum Pressure: -80KPa Rated Output Torque: 12mNm Blade Size: Φ5.0*390mm; Φ3.5*390mm Blade Work Mode: Corotation alternates reversal |
References
- Maliszewski, T. M., Sikorski, A. 574 Diode laser 980 nm for the treatment of BPH: Long-term comparison of the enucleation vs. vaporization. European Eurology. 14 (2), 137-151 (2015).
- Lerner, L. B., Rajender, A. Laser prostate enucleation techniques. Canadian Journal of Urology. 22 (Suppl 1), 53-59 (2015).
- Das, A. K., et al. A retrospective comparison of diode to holmium for laser enucleation of the prostate. Canadian Journal of Urology. 26 (4), 9836-9842 (2019).
- Hruby, S., et al. Eraser Laser Enucleation of the Prostate: Technique and Results. European Urology. 63 (2), 341-346 (2013).
- Lerner, L. B., Archana, R. Laser prostate enucleation techniques. Canadian Journal of Urology. 22 (5 Suppl 1), 53 (2015).
- Leonardi, R., Caltabiano, R., Lanzafame, S. Histological evaluation of prostatic tissue following transurethral laser resection (TULaR) using the 980 nm diode laser. Archivio Italiano di Urologia e Andrologia. 82 (82), 1-4 (2010).
- Kahokehr, A., Gilling, P. J. Enucleation techniques for benign prostate obstruction: Which one and why?. Current Opinion in Urology. 24 (1), 49-55 (2013).
- Chung, D. E., Te, A. E. New techniques for laser prostatectomy: an update. Therapeutic Advances in Urology. 1 (2), 85-97 (2014).
- Wu, G., et al. A comparative study of diode laser and plasmakinetic in transurethral enucleation of the prostate for treating large volume benign prostatic hyperplasia: a randomized clinical trial with 12-month follow-up. Lasers in Medical Science. 31 (4), 599-604 (2016).
- Wang, X., et al. Photoselective Vaporesection of the Prostate via an End-firing Lithium Triborate Crystal Laser. Journal of Visualized Experiments. (135), e57336 (2018).
- Shigemura, K., Tanaka, K., Yamamichi, F., Chiba, K., Fujisawa, M. Comparison of Predictive Factors for Postoperative Incontinence of Holmium Laser Enucleation of the Prostate by the Surgeons’ Experience During Learning Curve. International Neurourology Journal. 20 (1), 59-68 (2016).
- Stroman, L., Ellis, D., Toomey, R., Mazaris, E. An 18-month Audit of TURP Complications using the Clavien-Dindo Classification System. Journal of Urology. 1 (3), 3 (2013).
- Li, B., Xu, A., Zou, Y., Liu, C. A Randomized Trial Comparing Diode Laser Enucleation of the Prostate with Plasmakinetic Enucleation and Resection of the Prostate for the Treatment of Benign Prostatic Hyperplasia. Journal of Endourology. 27 (10), 1254-1260 (2013).
- Lerner, L. B., Rajender, A. Laser prostate enucleation techniques. Canadian Journal of Urology. 22 (5 Suppl 1), 53 (2015).
- Wu, G., et al. A comparative study of diode laser and plasmakinetic in transurethral enucleation of the prostate for treating large volume benign prostatic hyperplasia: a randomized clinical trial with 12-month follow-up. Lasers in Medical Science. 31 (4), 599-604 (2016).
- Xu, A., et al. A randomized trial comparing diode laser enucleation of the prostate with plasmakinetic enucleation and resection of the prostate for the treatment of benign prostatic hyperplasia. Journal of Endourology. 27 (10), 1254-1260 (2013).
- Yang, S. S., Hsieh, C. H., Lee, Y. S., Chang, S. J. Diode laser (980 nm) enucleation of the prostate: a promising alternative to transurethral resection of the prostate. Lasers in Medical Science. 28 (2), 353-360 (2013).
- Liu, L., Cheng, F., Li, H., Yu, W., Rao, T. Comparison of Clinical Effect Between Transurethral 1 470 nm Diode Laser Enucleation of the Prostate and Transurethral Bipolar Plasmakinetic Resection of Prostate. Medical Journal of Wuhan University. 39 (5), 809-812 (2018).
- Nair, S. M., Pimentel, M. A., Gilling, P. J. A Review of Laser Treatment for Symptomatic BPH (Benign Prostatic Hyperplasia). Current Urology Reports. 17 (6), 1-8 (2016).
- Cho, M. C., et al. Predictor of de novo urinary incontinence following holmium laser enucleation of the prostate. Neurourology, Urodynamics. 30 (7), 1343-1349 (2011).
- Herrmann, T. R. Long-term outcome after endoscopic enucleation of the prostate: From monopolar enucleation to HoLEP and from HoLEP to EEP. Der Urologe. Ausg. A. 55 (11), 1446 (2016).

.
