Examen cardiaque III: Bruits cardiaques anormaux
English
Share
Overview
Source : Suneel Dhand, MD, médecin, médecine interne, Beth Israel Deaconess Medical Center de fréquentant
Une connaissance fondamentale des bruits cardiaques normaux est la première étape pour distinguer le normal de l’anormal. Les murmures sont des sons qui représentent le flux sanguin turbulent et anormal à travers une valvule cardiaque. Elles sont causées par une sténose (zone de la valve trop étroit) ou régurgitation (reflux sanguin à travers la valve) et sont communément entendus comme un bruit de « sifflement » lors de l’auscultation. Les murmures sont notés de 1 à 6 en intensité (1 étant le plus doux et 6 le plus fort) (Figure 1). Les murmures cardiaques plus communs entendus sont côté gauche les murmures des valves aortiques et mitrales. Côté droit les murmures des valves tricuspides et pulmonaires sont moins fréquentes. Les murmures sont entendus généralement plus fort à la région anatomique qui correspond à la pathologie valvulaire. Souvent, ils rayonnent également à d’autres domaines.
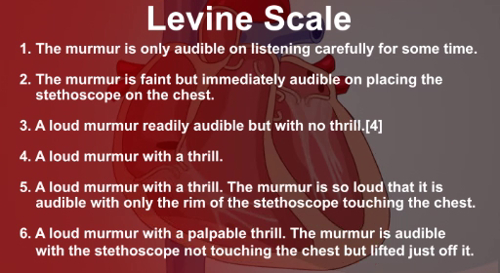
La figure 1. L’échelle de Levine utilisée à intensité de murmure de grade.
Outre les deux sons coeur principale, S1 et S2, qui sont normalement produites par la fermeture des valves du coeur, il y a deux autres sons cardiaques anormales, appelées S3 et S4. Ce sont également connu sous le nom galops, en raison de la nature « au galop » de plus de deux sons dans une rangée. S3 est un son grave entendu au début de la diastole, causée par le sang dans le ventricule. S3 est un signe d’insuffisance cardiaque avancée, mais il peut être normal chez certains patients plus jeunes. S4 est entendu fin diastole et représente le remplissage ventriculaire en raison de la contraction auriculaire en présence d’un ventricule rigide. S4 est également entendu dans l’insuffisance cardiaque et une hypertrophie ventriculaire gauche.
Procedure
Applications and Summary
The ability to recognize and distinguish between the different cardiac murmurs develops with time and practice. The first step is to identify normal from abnormal. When a murmur is heard, an examiner should think about the following questions: What part of the cardiac cycle does it occur in – systolic or diastolic? Where is the murmur loudest? Where does the murmur radiate to? Is it loudest on inspiration or expiration?
An examiner should make sure the environment is quiet and that there is ample time to hear the murmur. Loud murmurs are often heard across the precordium, in which case, ascertaining where it is loudest and where it radiates to is crucial. Whenever a murmur is heard, the clinician should get into the habit of going through this systematic approach in order to correctly diagnose the underlying pathology.
Transcript
Having a fundamental understanding of normal and abnormal heart sounds is the first step toward distinguishing between them. Murmurs and gallops present two broad categories of abnormal heart sounds. Murmurs are sounds that represent turbulent and abnormal blood flow across a heart valve. On the other hand, gallops refer to the occurrence of more than two heart sounds in a row.
In this video, we’ll first review the phonocardiograms of, and the mechanism behind different abnormal heart sounds. Then, we’ll discuss the auscultation landmarks and the essential steps useful for identifying underlying cardiac pathologies
Murmurs are caused either by stenosis, that is valve area narrowing, or due to regurgitation, which refers to the backflow of blood across a valve. However, not all murmurs are pathological; systolic murmurs can be benign in younger people.
All murmurs are categorized according to the intensity or loudness, pitch-high or low, harsh or blowing, configuration-crescendo decrescendo, location, and timing in the cardiac cycle-systolic or diastolic. The murmur intensity is graded from 1 to 6 on the Levine scale, 1 being the softest referring to the murmur only audible on listening carefully for some time, and 6 refers to the loudest murmur with a palpable thrill, which is audible with the stethoscope not touching the chest but lifted just off it.
The most common cardiac murmurs heard are the left-sided murmurs of the aortic and mitral valves. Aortic stenosis is a harsh-sounding, systolic, crescendo-decrescendo murmur that sounds like this… This murmur classically radiates to the carotid arteries and can be heard in the carotid area of the neck. The murmur of aortic regurgitation is a soft-blowing, early diastolic, decrescendo murmur; take a listen… On the other hand, mitral regurgitation is a blowing, pansystolic or holosystolic murmur that sounds like this… This murmur usually radiates towards the axilla. Lastly, mitral stenosis produces a low frequency, rumbling, and mid-diastolic murmur… The right-sided murmurs, which are related to the tricuspid and pulmonary valves, are rare. Additionally, hypertrophic cardiomyopathy, which is a genetic disorder leading to an abnormal thickening of the cardiomuscular wall, produces a systolic, crescendo-decrescendo murmur… Likewise, Patent Ductus Arteriosus-a congenital heart disorder in which the ductus arteriosus does not close-induces a continuous machine-like murmur…
Except murmurs, other atypical heart sounds include gallops S3 and S4. This is the S3 gallop…which is a low-pitched sound, heard in early diastole, caused by blood entering the ventricle. Whereas S4, which sounds like this…is heard in late diastole, and represents ventricular filling due to atrial contraction in the presence of a stiff ventricle. S3 is a sign of advanced heart failure, although it can be normal in some younger patients. And S4 is also heard in heart failure and in presence of left ventricular hypertrophy.
In addition to murmurs and gallops, splitting of normal heart sounds may occur. Each normal heart sound-S1 and S2-is composed of two components referring to the closing of the two valves, which make up that sound. Therefore, S1 is composed of tricuspid T1 and mitral M1 components. Similarly, S2 is composed of aortic A2 and pulmonary P2 elements. It’s hard to distinguish between the sounds produced by individual valves, as they close almost together. But if the pair of valves is not closing together, then a “split” might appear on auscultation.
S2 split during inspiration that sounds like this…is normal. It is referred to as the “physiological” split. However, if S2 split occurs during expiration, it called “paradoxical” split…which occurs when there is a prolonged left ventricular phase, such as in left bundle branch block or hypertrophic cardiomyopathy. And if the split occurs throughout the respiratory cycle, then it is known as “fixed” split…which can be heard in case of an atrial septal defect.
The last abnormal heart sound that we’ll discuss is a result of pericarditis, which refers to inflamed pericardium. The sound is known as the “friction rub”, which occurs due to the rubbing of the inner and outer pericardium layers against each other
Now that we have reviewed the normal and abnormal heart sounds, let’s discuss the auscultation steps essential to distinguish them from one another. Remember, each murmur is usually heart loudest at the anatomical area that corresponds to the valvular pathology
When auscultating to specifically diagnose a murmur, ask the patient to breathe in and out deeply, as the murmur timing in the respiratory cycle can provide a vital diagnostic clue. Start by placing the diaphragm in the aortic area to detect murmur due to aortic stenosis. If present, auscultate the carotid area as this murmur classically radiates to this neck region. Always listen for at least 5 seconds to ensure that you’re not missing any subtle sounds. To detect murmur due to aortic regurgitation, request the patient to lean forward. Remind the patient to breath in and out constantly. Now, using the diaphragm, auscultate at the lower left sternal border, close to the tricuspid area. This is done to accentuate the murmur of aortic regurgitation. In the same position, if pericarditis is present, you might encounter sounds due to the friction rub.
Next, request the patient to lie back and using the diaphragm, listen to the sound in the mitral area to identify mitral regurgitation. If present, move the stethoscope laterally to confirm radiation to the axilla. In addition, using the bell of the stethoscope, auscultate the mitral area to check for the presence of mitral stenosis. Subsequently, using the diaphragm auscultate the pulmonic area. Here, you can clearly distinguish the second heart sound and sometimes you may hear the S2 split. Note at which phase of respiratory cycle the splitting occurs, as this can help in classifying the split as physiological, paradoxical or fixed. In addition, you may encounter the systolic murmur due to pulmonary stenosis or a diastolic one due to pulmonary regurgitation.
Next, auscultate the tricuspid area. Here, similar to the pulmonic area, you may come across the murmurs associated with tricuspid regurgitation and stenosis, which are systolic and diastolic in nature, respectively. Next, instruct the patient to lie on their left side and with the bell pressed lightly on the patient’s chest, auscultate in the mitral and the tricuspid area. In this position, you might hear the murmur of mitral stenosis, as well as the galloping S3 and S4 sounds.
Additionally, if you suspect hypertrophic cardiomyopathy, then using the diaphragm, auscultate between the apex and left lower sternal border. If you hear a systolic, crescendo-decrescendo murmur in this area then you should request the patient to sit straight and perform the Valsalva maneuver. One of the ways to this is by asking the patient to blow out with mouth closed. This maneuver is known to accentuate the hypertrophic cardiomyopathy-associated murmur. Furthermore, if the rare patent ductus arteriosus or PDA is suspected, then auscultate the upper left chest region to listen for the characteristic continuous machine-like murmur.
You’ve just watched JoVE’s video on cardiac auscultation highlighting the abnormal heart sounds. In this video, we reviewed the phonocardiograms of commonly encountered abnormal heart sounds and the pathology behind their occurrence. We also highlighted the important steps that every physician should perform during cardiac auscultation so that the presence of abnormal sounds does not go undetected. As always, thanks for watching!
